Neuropathic Pain Can Be Evident Across Various Types of CMT
Neuropathic pain, related to damage or impairment in nerve receptors that detect pain and heat, is most common in CMT1A patients but can be found in people with different types of Charcot–Marie Tooth (CMT) disease, a study found.
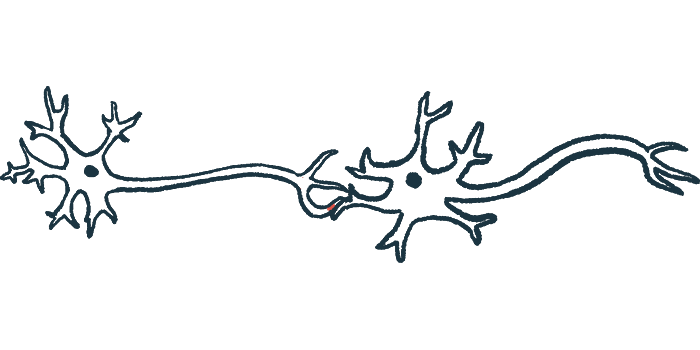
Abnormal electrical signals along nerve fibers in response to heat generated by lasers, known as laser-evoked potentials, were significantly associated with neuropathic pain. These signals may help in detecting nerve impairment in CMT patients, the researchers noted.
The study, “Neuropathic pain in Charcot–Marie-Tooth disease: A clinical and laser-evoked potential study,” was published in the European Journal of Pain.
CMT is a group of disorders involving the nerves that supply movement and sensation to the arms and legs, known as the peripheral nervous system. Its several types are classified based on inherence patterns, underlying genetic mutations, and how fast electrical impulses travel along nerves (nerve conduction speed).
The most common symptoms are progressive muscle weakness and the loss of muscle tissue, fatigue, walking difficulties, hearing loss, and a diminished sensation to heat, cold, or pain if sensory nerves are affected.
People with CMT may also experience neuropathic pain, characterized by tingling and burning pain sensations in the hands and feet. Emerging evidence suggests neuropathic pain is caused by damage to small nerve fibers that detect pain, temperature, and itching sensations in the skin.
Most previous studies investigating neuropathic pain have focused on CMT1A, the most common genetic CMT subtype. In this report, researchers in Italy explored neuropathic pain and small nerve fiber involvement in different CMT subtypes.
Their study enrolled 50 CMT patients, ranging in age from 13 to 72, and 41 healthy controls between the ages of 26 and 68.
Among the patients, 19 were diagnosed with CMT1A caused by defects in the PMP22 gene, and 12 with CMTX1 associated with mutations in GJB1. Eleven patients had CMT due to MPZ mutations: five were diagnosed with CMT1B, three with CMT2J, two with CMT2I, and one with CMTDID.
The remaining eight patients had MFN2 mutations, with six diagnosed with CMT2A and two with CMT2A2B.
Patients were asked to report pain and its location, and to rate their pain on a numeric scale ranging from 0 (no pain) to 10 (worst pain ever). A mean pain intensity of 6 was reported by 17 of these 50 people (34%), with pain more frequently reported by CMT1A patients and among women. No relationship was found between pain intensity and patients’ age.
Neuropathic pain was reported by seven participants (14%): five CMT1A patients, one with CMT2J and another with CMTX1. Its mean intensity was 6.67, and CMT1A individuals were more frequently affected than other groups. It was most common in the feet, followed by hands. Neuropathic pain was also not related to age.
Nociceptive pain, which feels sharp, aching, or throbbing and is generally caused by tissue damage, was more frequently located in the back, feet, and shoulders, and then the knees.
Patients were evaluated for laser-evoked potentials (LEPs), which are brain responses to laser radiant heat pulses and reflect the activation of A-delta nociceptors, or pain and heat receptors. LEPs are a standard technique for studying pain pathway function in people with neuropathic pain.
For this, people were seated in a comfortable chair, with their right hand and foot stimulated by heat from lasers. Electrodes recorded the resulting pain-related electrical signals traveling through nerves called N2 waves, which are part of the N2-P2 complex (full electrical signal).
Compared with controls, the mean latency — delay — in the N2 signal was significantly longer in the foot and hands of patients with MPZ mutations. Differences in the strength of electrical signals were observed between CMT subgroups and controls, but did not reach significance.
Abnormal LEPs with increased N2 latency in the foot were recorded in 11 of the 19 CMT1A patients. In patients with unusual LEPs, the mean signal strength was significantly lower in the foot, and the mean latency was significantly higher in the hand relative to those with normal LEPs.
All CMT1A patients with neuropathic pain had abnormal LEPs, as did some without neuropathic pain, “supporting the role of [A-delta] fibers dysfunction,” the team wrote.
Among people with MPZ-related CMT, two out of the four CMT1B patients showed prolonged N2 latency in the hand and foot. The remaining patients showed normal LEPs.
Among the 12 CMTX1 patients, 11 had normal LEPs. Men had a significantly lower mean strength of the full N2–P2 complex signal than did women, but they were within normal limits. One female patient reported neuropathic pain but with normal LEPs.
All eight patients with MFN2-related CMT had normal LEPs, and none reported neuropathic pain.
Statistical analysis confirmed a significant relationship between abnormal LEPs and neuropathic pain. Normal LEPs predicted the absence of neuropathic pain at a level of 96.6%.
Decreased N2–P2 complex strength in both the hands and feet correlated with higher (poorer) scores on the CMT neuropathy score second version (CMTNSv2), a scale to measure the level of disability and disease progression over time. No correlation was seen between latency and CMTNSv2 scores.
“[Neuropathic pain] is a frequent finding in common CMT1A, but it may occur also in other selected subtypes of CMT such as CMT2J and is highly related to [A-delta] fibers impairment,” the investigators concluded. “LEPs have a negative predictive value for [neuropathic pain], suggesting that the probability to develop [neuropathic pain] is low for a patient with [a] normal test.”
LEPs, the researchers added, “represent an important instrument that supports the neurologist in the management of CMT patients, addressing the best symptomatic treatment for pain.”