Orthopedic Shoes Can Improve Walking, But Not Stability, in Patients
Written by |

Africa Studio/Shutterstock
Compared to regular footwear, customized orthopedic shoes significantly improve walking, including speed, in adults with Charcot-Marie-Tooth (CMT) disease, according to a small study in the Netherlands.
However, no significant differences in postural stability while standing or walking were noted when patients wore orthopedic versus standard shoes.
While orthopedic footwear is commonly prescribed for CMT patients with balance or walking problems, these findings provide evidence of its beneficial effects on patients’ gait, or walking pattern, the researchers noted.
Larger studies are needed to assess the benefits of specific features of orthopedic shoes for CMT patients.
The study, “Effects of orthopedic footwear on postural stability and walking in individuals with Hereditary Motor Sensory Neuropathy,” was published in the journal Clinical Biomechanics.
CMT, also known as hereditary motor sensory neuropathy, comprises a group of inherited neuromuscular disorders affecting the peripheral nervous system, the network of nerves that control movement and sensation (touch, heat, cold) to the arms and legs.
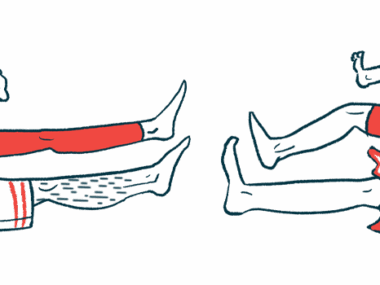
Due to muscular weakness, CMT patients often develop foot deformities and walking difficulties, such as foot drop. Foot drop refers to when a person cannot lift their toes normally when taking a step, making them drag their feet on the ground, which increases the risk of falls.
CMT patients commonly have postural instability and walk slower, take smaller steps (shorter step length), and wider steps (increased step width, or lateral distance between the two feet) than people without walking impairments.
As such, orthopedic footwear is commonly prescribed for people with CMT. Low orthopedic shoes aim to improve foot loading by compensating for foot deformities, while high orthopedic footwear “may additionally compensate for weakness of the lower leg muscles during walking,” the researchers wrote.
However, there is limited evidence of the efficacy of orthopedic footwear in people with CMT.
To address this, a team of researchers in the Netherlands, along with a colleague in Belgium, evaluated the effects of customized orthopedic footwear on postural stability and walking patterns of 15 adults (10 men and five women) with CMT seen at a single Dutch center.
Customized orthopedic footwear for CMT usually includes an insole designed to accommodate the foot deformity to relieve pain and pressure, and improve the hindfoot position. External footwear features, such as shaft height, heel adjustment, and the position where the outsole begins to curve upwards, are based on a patient’s characteristics, such as muscle strength and gait, and on the treatment purpose.
Patients, with a mean age of 49.6 years, had their customized orthopedic shoes for at least two months. All used the shoes for eight or more hours per day and all but one for six to seven days a week. Most of the shoes were of mid-height, and had a beveled heel, and an early outsole upward curve.
Participants performed a quiet standing task (with eyes either open or closed) and a two-minute walking test while they wore their customized orthopedic shoes and standard, minimally supportive, flexible sneakers (to minimize influence on gait).
Patients underwent practice walking trials to familiarize themselves with the standardized sneakers. Postural and gait data were collected through 20 markers placed on the footwear.
Results showed that customized orthopedic shoes had no significant effect on postural stability during standing or walking relative to standard sneakers. However, customized footwear significantly improved several gait parameters, with patients walking faster and taking longer and narrower steps than when using standard shoes.
While patients continued to walk slower than most people, 86.7% showed an increase in gait speed higher than 0.10 meters per second, which is considered clinically relevant.
“Improved heel landing at initial contact for all orthopedic footwear and reduced foot drop during swing for mid and high orthopedic footwear seemed to be the main contributors to gait improvement when wearing orthopedic footwear,” the researchers wrote.
These findings suggest that orthopedic footwear improves gait in adults with CMT, but does not affect their postural stability during standing or walking.
“This is the first study to support its beneficial effects on the gait pattern in a larger group of affected individuals,” the team wrote.
Given the small number of patients included in the study, the researchers were unable to assess the effects of individual orthopedic footwear features on specific gait parameters. Therefore, future, larger studies are needed to evaluate such potential links.