Nerve Cells in CMT2P Slowly Recover From Injury, Study Suggests
Findings in mice may help explain progression in patients, but raise 'challenge'

Repeated damage to nerve cells, also called neurons, may explain in part why symptoms appear to develop slowly in patients with a form of Charcot-Marie-Tooth disease type 2 (CMT2) called CMT2P, a study in a mouse model suggests.
Researchers suggested this to explain why neurons in mice carrying a known disease-causing mutation did not waste away, but took longer to recover after an injury.
While the delay was subtle, study findings provide “a helpful clue” toward understanding how CMT2P occurs and develops over time.
“As every person is exposed to many nerve injuries during their lifetime, we speculate that an accumulation of impaired nerve recoveries may eventually contribute to the polyneuropathy of CMT2P,” the researchers wrote, while noting that mice might not be an ideal model for nerve studies in this disease.
The study, “C698R mutation in Lrsam1 gene impairs nerve regeneration in a CMT2P mouse model,” was published in the journal Scientific Reports.
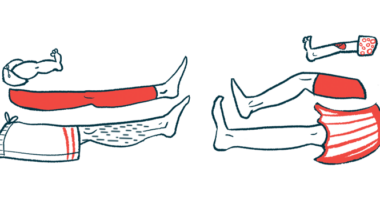
CMT2 occurs as the axons of multiple peripheral neurons (those outside of the brain and the spinal cord) become damaged at the same time. (An axon, or nerve fiber, is the slender projection of a neuron that carries electrical signals away from the cell’s body to the next neuron or muscle cell.)
The damage causes muscles to weaken and waste away. Disease symptoms usually begin in the feet and legs and gradually move up along the limbs, worsening over time.
Study in how LRSAM1 mutation affects nerve cells
CMT2P, one of the many forms of CMT2, is caused by mutations in a gene called LRSAM1, which provides the instructions for making an E3 ubiquitin ligase, a type of protein that tags other proteins for recycling within cells. This helps keep cells healthy by clearing away unwanted or poorly working proteins.
One LRSAM1 disease-causing mutation is C694R, which is known to prevent E3 ubiquitin ligase from properly tagging the other proteins for recycling. As in other forms of CMT2, its symptoms take off in the second or third decade of life and may appear mild before slowly getting worse over time.
To better understand how C694R causes CMT2P, researchers in the U.S. engineered mice to carry that mutation in one or both copies of the Lrsam1 gene, the mouse equivalent of LRSAM1.
To do this, they turned to CRISPR/Cas9, a kind of molecular scissors that can be used to manipulate DNA and leave open a gap where new building blocks can be added. The new building blocks the team added were the faulty, or mutated, ones.
When the mice were 6 to 12 months of age, roughly equivalent to people in their 30s or 40s, the researchers tested the animals’ motor function.
Mice carrying the mutation in one or both copies of the Lrsam1 gene clasped their back limbs in a similar way to healthy (wild-type) mice when held by the tail. They also hung on to a rotating rod, called a rotarod, for a similar amount of time. These findings suggested that mice carrying the mutation had normal motor function.
A nerve conduction velocity test revealed that electrical signals traveled through the sciatic nerve of mutated mice as fast as through those of wild-type mice up to the age of 30 months, an equivalent to the elderly in people. The sciatic nerve is a long nerve that runs from the lower back and down each leg.
A closer look found that the sciatic nerve contained as many axons in mutated mice as in wild-type mice. It also contained as much myelin, a fatty substance that forms around axons to protect them and allows them to fire electrical signals effectively.
In line with these findings, the mutated protein was able to interact with RNA-binding proteins, a key step for its tagging job.
“This mild phenotype [disease-related characteristics] is in line with absent disruption of protein–protein interactions between mutant LRSAM1 and RNA-binding proteins,” the researchers wrote.
But why this interaction continued was “unclear” and raised a “challenging issue,” the team added. “The nerve abnormality in the knock-in mice was disproportionally subtle, comparing with the polyneuropathy in persons with CMT2P.”
To better mimic what happens in humans, “perhaps CMT2P needs to be modeled in larger animals” than mice, the scientists wrote.
To find out whether neurons in mutated mice were able to recover from injury as rapidly as those in wild-type mice, the researchers crushed their sciatic nerve and then measured nerve conduction velocity. They found that the sciatic nerve of mutated mice fired slower electrical signals after injury.
The differences were subtle, however. Overall, the C698R mutation “only mildly impaired nerve function during regeneration,” the researchers wrote.
“Repetitive nerve injuries may, at least partially, contribute to the slowly progressive axonal loss in CMT2P,” they concluded.