Blocking SIRT2 Enzyme Shows Promise as Potential CMT2D Therapy

Matej Kastelic/Shutterstock
Mutations in the GARS protein — found in people with Charcot-Marie-Tooth disease type 2D (CMT2D) — enhanced the activity of the enzyme SIRT2, and led to motor deficits and other alterations in fruit flies, a study has found.
In turn, blocking the action of SIRT2 rescued motor deficits, supporting its potential as a therapeutic target to treat CMT2D.
The study, “SIRT2-knockdown rescues GARS-induced Charcot-Marie-Tooth neuropathy,” was published in the journal Aging Cell.
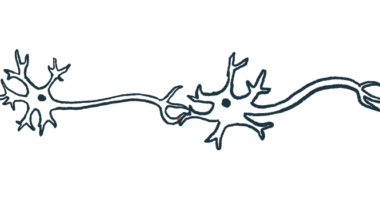
CMT2 is caused by genetic defects that alter the function of peripheral nerve fibers (axons), which are important for muscle control and sensation.
The disease subtype CMT2D is caused by mutations in the GARS gene, which encodes the enzyme glycyl t-RNA synthetase. This condition is characterized by weakness in the hands starting in adolescence or early adulthood and progressive muscle weakness and shrinkage, among other alterations.
However, it remains unclear how GARS genetic defects impair the ability of axons to transmit electrical nerve impulses.
The enzyme sirtuin 2 (SIRT2) is responsible for removing chemical acetyl groups from alpha-tubulin, a protein that, together with beta-tubulin, forms microtubules — long tube-like structures that provide structure and shape to cells.
Acetyl groups on alpha-tubulin help stabilize microtubules. A well-organized microtubular network is necessary for the proper function of cells, including nerve cells. Studies suggest SIRT2 may be a potential therapeutic target to treat neurodegenerative conditions such as Parkinson’s disease and Huntington’s disease.
These findings prompted researchers based at Fudan University in China to wonder whether there was a connection between the SIRT2 and GARS proteins that may help explain how GARS gene mutations lead to axon defects that cause CMT2D.
First, the team showed that, within motor nerve cells (neurons), normal GARS protein, or wild-type GARS, bound to SIRT2 but not SIRT1, another Sirtuin family member in the cell.
Motor neurons were then created to produce normal GARS as well as two GARS proteins that carry CMT2D-related changes — GARS-G526R and GARS-E71G. Normal GARS was able to bind more with SIRT2 than the CMT2D-related mutants. In cells that produced both SIRT2 with normal GARS and mutant GARS, the enzyme interacted tightly with normal GARS but not with the CMT2D mutants.
Purified versions of SIRT2 and GARS were made to test whether the interaction of these proteins would directly affect the ability of SIRT2 to remove acetyl groups (deacetylase activity). Results showed that GARS significantly decreased SIRT2 activity in a dose-dependent manner. But, the same concentrations of GARS-CMT2D mutants barely blocked this activity.
Next, mixing the motor neuron components containing SIRT2 with increasing concentrations of normal and mutant GARS, the team found a significant dose-dependent increase in the addition of acetyl groups (acetylation) of alpha-tubulin with normal GARS, but not with the CMT2D mutants. A similar effect was seen when normal GARS2 was overproduced in cells.
“These data indicate that the interaction of wild-type GARS and SIRT2 inhibits the deacetylase activity of SIRT2 and leads to the acetylated [alpha]-tubulin, which might protect microtubules from mechanical breakage,” the researchers wrote.
In contrast, as GARS mutations were unable to stop the SIRT2-dependent removal of acetyl groups from alpha-tubulin, this may destabilize microtubules and explain how these mutations lead to nerve cell malfunction seen in CMT2D.
An examination of the normal GARS protein structure found that CMT2D-related mutations were in a position to disrupt the proper binding with SIRT2.
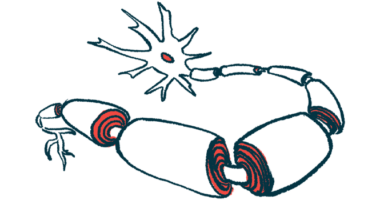
Finally, these results were tested in a fruit fly (Drosophila) model of CMT2D, which carried the GARS-G526R mutation and demonstrated motor performance deficits when compared to flies with normal GARS. These flies with the CMT2D-associated mutation also have a dramatic decrease in the number of neuromuscular junctions — the place where nerve and muscle cells communicate.
The GARS-G526R flies had difficulties climbing, but genetic suppression of SIRT2 restored climbing ability similar to control flies.
Adding a molecule called AGK2, which specifically blocks the activity of SIRT2, gradually rescued the climbing deficits seen in GARS-G526R flies in a time-dependent manner. Further, by genetically suppressing SIRT2 in flies with GARS-G526R, the scientists found a significant increase in the number of neuromuscular junctions and acetylated tubulin.
“Overall, these results strongly indicate that the inhibition of SIRT2 could rescue the motor performance deficits in GARS-mutant CMT flies in a Drosophila model,” the researchers added.
Consistently, reducing the activity of GARS-G526R, or blocking the action of SIRT2, significantly extended the life span of GARS-G526R flies.
“Our study provides another promising strategy to treat the peripheral neuropathy [nerve damage] resulting from CMT by inhibiting SIRT2, suggesting that the targeting of SIRT2 might have a general beneficial impact on neurodegenerative diseases,” the investigators wrote.