HDAC6 Protein Likely Treatment Target in CMT2D, Study Suggests
Treatment with CKD504, an inhibitor of the protein HDAC6, enhanced the activity of spinal cord neurons genetically engineered to harbor mutations in the GARS1 gene, a study found. Mutations in GARS1, which disrupt nerve signals, cause Charcot-Marie-Tooth disease type 2D (CMT2D).
Together with other benefits, these findings highlight CKD504 as a potential treatment for CMT2D, according to researchers.
The study, “HDAC6 Inhibition Corrects Electrophysiological and Axonal Transport Deficits in a Human Stem Cell-Based Model of Charcot-Marie-Tooth Disease (Type 2D),” was published in the journal Advanced Biology.
CMT, one of the most common inherited disorders, is caused by mutations that impact the function of nerves found outside the brain and spinal cord, also known as peripheral nerves. These nerves control movement and sensation by transmitting information between the brain and the rest of the body.
People with CMT2D carry mutations in the GARS1 gene, which provides the instructions for the enzyme GlyRS. Studies in mice have associated mutations in the GARS1 gene with malformations in the neuromuscular junctions — the locations where nerve and muscle cells communicate — issues with muscle contraction, and decreases in nerve conduction velocities. However, the exact mechanism of how GARS1 mutations cause CMT2D is unknown.
Now, a team of researchers in the U.S. and the Republic of Korea developed a human cell line of motor neurons with GARS1 mutations and evaluated its use as a model to test compounds for the treatment of CMT2D.
A gene-editing tool called CRISPR/Cas9 was used to induce specific GARS1 mutations in human stem cells that were then differentiated into motor neurons.
To investigate the electrical properties and activity of these motor neurons, a whole cell patch clamp analysis was performed. However, no significant differences were found between GARS1 mutant neurons and the controls. The scientists were not surprised by these results since, in CMT2D, defects are thought to occur at the end of nerve fibers and this technique picks up electrical activity from the cell body.
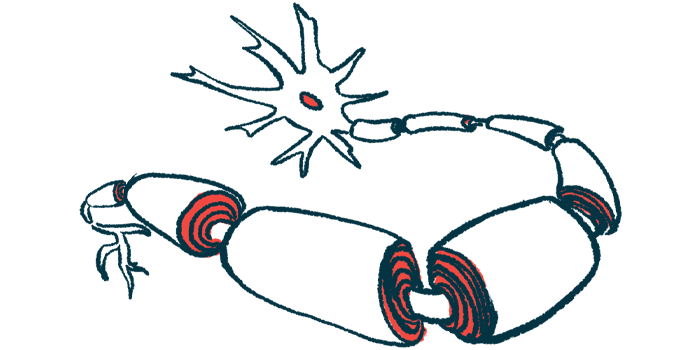
In nerve fibers, motor proteins direct hollow rods — called microtubules — to move lipids (fat-like molecules), proteins, and organelles such as mitochondria, which are responsible for energy production in cells. Microtubules are formed by alpha-tubulin, which needs to be acetylated, or modified, for proper function. Therefore, protein levels of acetylated alpha-tubulin were analyzed in GARS1 mutant cells. The findings showed that acetylated alpha-tubulin levels in GARS1 mutant neurons were 18.4% lower than in controls.
Previous research indicated that mutant GlyRS proteins in mice interact abnormally with the HDAC6 protein. Abnormal GlyRS-HDAC6 interactions lead to lower acetylation of alpha-tubulin. In their next set of experiments, the researchers tested the effects of CKD504, an HDAC6 inhibitor developed to treat Huntington’s disease.
“HDAC6 is an attractive drug target for CMT2 given the significant amount of evidence for the therapeutic efficacy of HDAC6 inhibition in modulating neurodegenerative disease [manifestations],” the team wrote.
When human motor cells with a GARS1 mutation were treated with CKD504, or tubastatin A (another HDAC6 inhibitor), acetylated alpha-tubulin levels increased to levels higher than in untreated controls. In addition, further assays confirmed that mutant GARS proteins formed abnormal complexes with HDAC6 in cultured human cells.
Analysis of mitochondrial movement showed that these organelles move more slowly in GARS1 mutant nerve fibers compared with controls. Treatment with higher concentrations of tubastatin A and CKD504 significantly increased mitochondrial velocities.
Next, activity patterns were investigated using multielectrode arrays or MEAs. Unlike whole cell patch clamp, which analyzes single cells, MEAs can detect activity in an entire population of cells. Using this method, the researchers were able to observe that spontaneous activity in spinal cord neurons with GARS1 mutations was decreased compared with controls. The mean firing rate, as well as the number of bursts, also were lower in neurons with mutations. Of note, firing rate and bursting are indicators of activation in neurons.
CKD504 had a positive effect on spontaneous firing rates in both mutant cells and controls. According to scientists, HDAC6 inhibition probably promotes general neuronal stability.
“Taken together, these MEA data suggest that improved axon [nerve fiber] stability and mitochondrial transport due to HDAC6 inhibition has a positive impact … in GARS1 mutant neurons,” the investigators wrote.
The results were further validated in a patient-derived cell line with a GARS1 mutation. The patient, with a mutation that had never been reported before, had classic symptoms of CMT2D, including muscle weakness and high foot arch. He had moderate to severe clinical disabilities, according to appropriate scales.
Treatment with CKD504 significantly improved the levels of spontaneous firing and burst activity in the patient-derived motor neurons.
“The consistent improvement in electrophysiological function [electrical activity] observed in CRISPR-edited and patient derived CMT2D neurons treated with CKD504 underscores the therapeutic potential of this compound for the future treatment of this condition,” the researchers wrote.
“The novel HDAC6 inhibitor CKD504 appears to be a suitable candidate for further development as a CMT2D-focused therapy,” they concluded.