Ultra Rare CMT Subtype 2Z Identified in 4 Chinese Families
Scientists in China examined the relationship between genetic mutations in the MORC2 gene and the various disease characteristics in people with the rare Charcot-Marie-Tooth disease subtype 2Z (CMT2Z).
Physicians should consider their study’s findings when working to diagnose unresolved cases showing muscle weakness and sensory problems in the outer limbs, its scientists wrote.
The study, “Characterization of genotype-phenotype correlation with MORC2 mutated Axonal Charcot–Marie–Tooth disease in a cohort of Chinese patients,” was published in the Orphanet Journal of Rare Diseases.
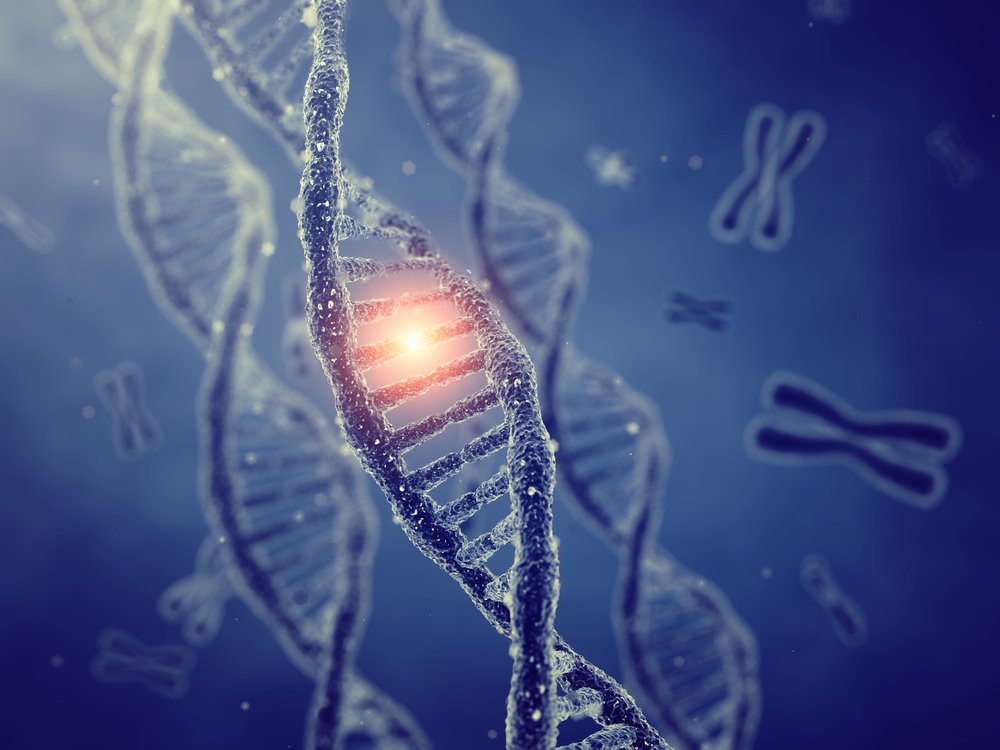
CMT2 is a type of CMT with genetic changes that disrupt the function of axons (nerve fibers) of the peripheral nerves, those outside the brain and spinal cord, that relay information between the brain and the rest of the body. CMT2 is also known as axonal CMT.
CMT2 subtype Z (CMT2Z) is caused by mutations in the MORC2 gene, which carries instructions for an enzyme thought to be involved in many functions, including DNA repair and the regulation of gene activity.
This CMT subtype impacts nerve fibers farthest from the spinal cord, and carries a wide range of characteristics. Some patients show weakness in infancy, while others have adult-onset weakness that may include upper and lower limb muscles, as well as sensory loss.
Only 10 different MORC2 mutations have been reported from 33 families in Spain, Australia, Germany, Czech Republic, Japan, South Korea, and China.
As such, the relationship between genetic defects and outward characteristics of the disease — referred to as a genotype-phenotype correlation — remains poorly understood.
Researchers based at three hospitals in China conducted a genetic analysis of a group of Chinese patients with unexplained axonal CMT.
The study enrolled 356 people from 284 unrelated Chinese CMT2 families. Blood was collected, and DNA was extracted and analyzed. Results identified four different mutations with MORC2-related disease in four unrelated families.
Family 1 had the previously unreported mutation c.1397A>G, in which A refers to adenine and G means guanine in the DNA sequence. This mutation occurred in affected family members, but not in unaffected healthy members.
This family included 10 affected and eight unaffected members over five generations. The first member identified was a 46-year-old woman who had progressive upper and lower limb weakness for 10 years. At 36, she noticed numbness in both hands and, over time, had more difficulties with daily activities. By age 40, she had trouble walking and lost sensation in her feet.
A neurological examination in the 46-year-old woman revealed prominent muscle atrophy (shrinkage) and weakness in the outer legs and hands, with moderate loss of sensation. While blood counts were normal, her creatine kinase levels were elevated, a sign of muscle injury. Her 19-year-old son had similar but milder symptoms.
Electrophysiological studies, which measure electrical signals along nerve fibers, showed motor and sensory nerve damage, or neuropathy. An MRI of calf skeletal muscles showed multiple abnormal signs, with fatty infiltration due to muscle loss.
Overall, individuals with this mutation had similar symptoms, including numbness and weakness in the outer limbs, with hand weakness appearing before that of the outer lower limbs. While some could walk without assistance, others’ walking abilities were limited and one patient was wheelchair dependent.
In family 2, the spontaneous, non-inherited mutation c.260C>T was identified, in which C refers to cytosine and T to thymine in the DNA sequence. This mutation was previously reported in one Spanish and two Korean patients with disease characteristics similar to the neurodegenerative disorder spinal muscular atrophy (SMA).
The first individual identified was a 7-year-old girl with no family history of genetic disease. She began to show delays in body movements at 8 months old, and could not crawl or walk at 16 months. By age 2, she could walk with assistance, and by 7 was mostly using a wheelchair and needed a walker.
A neurological exam showed she growth deficits and developmental delays. She had generalized weakness, including of the face and lips, and reduced muscle tone. She had muscular weakness in the upper and lower limbs along with scoliosis (spinal curvature), clawed hands, and flat feet. Sensory impairment was mild.
An electrophysiological study at 7 years old showed motor and sensory neuropathy, while an MRI showed brain abnormalities. Nerve biopsy revealed a loss of large nerve fibers with myelin, a fatty coating on axons that supports electrical signals.
In family 3, the spontaneous mutation c.754C>T was confirmed in twin sisters but not in their parents or brother. This mutation was the most commonly reported in other countries, but this study documented its first appearance in the Chinese population.
The twins were 10 years old at the time of this analysis. One sister showed development delays. At age 2, while she was able to walk, she could not run like others her age. She developed walking problems and foot deformities, and outward muscle atrophy by age 4. Although her twin developed normally, foot deformities and walking difficulties evident at age 6.
Neurological exams found typical growth and cognitive abilities. However, muscle strength in the 10-year-olds’ lower limbs was weakened with mild sensory impairment. Electrophysiological studies in both revealed motor neuropathy.
The mutation identified in family 4 was c.1220G>A, and was only found in a 19-year-old patient but not his parents or sister. It had also been reported in a Japanese patient.
The teenager had motor difficulties at 6 years of age. He was able to walk but ran slower than other children of the same age.
Disease progressed rapidly, and by 12, he had weakness and atrophy in the lower limb muscles. At 17, he could only walk a short distance without assistance, was unable to squat or stand up, and reported poor handwriting and difficulties dressing.
An examination revealed muscle weakness and atrophy in the lower limbs, with a foot deformity. He showed decreased sensation, as well as motor and sensory neuropathy.
“In conclusion, we described four Chinese axonal CMT families caused by MORC2 mutations,” the researchers wrote. “It should be considered in the diagnostic workup of unresolved cases of axonal neuropathy, SMA-like syndrome, and with other complex associated phenotypes [characteristics].”
Further research “may elucidate the mechanism underlying the diversity of MORC2-related diseases,” they added.