Theophylline Enhances Myelin Production in CMT1A Mice

Theophylline, a medication used to treat asthma and other respiratory conditions, promoted myelination — the process by which sheaths of myelin, a fatty substance, are produced around nerves to protect them — in a mouse model of Charcot-Marie-Tooth disease type 1 subtype A (CMT1A), a study shows.
Treatment with a short-term low dose of theophylline also improved motor coordination and led to partial recovery in CMT1A mice.
“Hence, Theophylline should be further evaluated as a potential new therapeutic approach to sustainably treat demyelinating peripheral neuropathies such as CMT1A,” the scientists wrote.
The study, “Theophylline Induces Remyelination and Functional Recovery in a Mouse Model of Peripheral Neuropathy,” was published in the journal Biomedicines.
The most common cause of CMT1A is the overproduction of PMP22 protein, a component of myelin, due to a genetic alteration. Myelin is produced by Schwann cells in peripheral nerves (outside the brain and spinal cord). Loss of myelin results in axonal degeneration — peripheral nerve damage — muscle weakness and wasting, and reduced sensation in the extremities.
Since too much PMP22 affects the structure of myelin and causes Schwann cells to die, many treatment strategies are directed at lowering the expression of this protein. However, the authors of this study tried a different approach — inducing remyelination of nerve fibers with Schwann cells to recover motor function.
Their previous studies showed that treatment with theophylline, a compound naturally found at low doses in tea leaves and cocoa beans, increased myelination in a mouse model of peripheral nerve injury by boosting the activity and expression of HDAC2, an important regulator of myelin proteins such as myelin protein zero (P0).
Now this team, based in Switzerland, investigated the effects of theophylline in a mouse model of CMT1A called C22. Mice were given either theophylline or saline for four days.
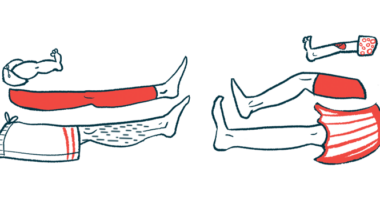
Twenty-one days after the treatment a coordination test was conducted. Mice were placed on a cage grid, which then was inverted to determine how long they were able to stay attached to the grid. Researchers also counted the number of grabs and missed steps.
Results showed that treated C22 mice had more successful grabs of the grid and fewer missed steps compared to the saline group. However, the average time C22 mice were able to hang on to the grid and the total number of steps were similar between the two groups. According to the scientists, these findings likely indicate no differences in muscle strength.
“A possible explanation could be that building up muscles takes a longer time and is strongly dependent on exercise, which may be restricted within the cage,” the authors wrote.
The number of myelinated fibers then was assessed in the sciatic nerves — the long nerves that run from the lower back down through the legs. Differences between treated and non-treated mice were found only in the large-caliber nerve fibers. While in treated mice the majority of these fibers were wrapped by a thin myelin sheath, in the control mice most large-caliber fibers had no myelin.
Researchers noted that no changes in myelin thickness were observed, “indicating that the treatment with Theophylline induced (re)myelination of large-caliber axons [nerve fibers] but did not affect myelin thickness of already myelinated axons.”
Further analysis revealed that the protein levels of P0 were significantly increased in the sciatic nerve tissues of C22 mice treated with theophylline compared to those treated with saline.
“This pilot study suggests that Theophylline treatment could be beneficial to promote myelination and thereby prevent axonal degeneration and enhance functional recovery in CMT1A patients,” the authors concluded.