Electrical Nerve Stimulation Eases CMT1A Mice Myelin Loss, Symptoms
Researches said approach 'lays the groundwork' for electroceutical treatment

Electrical stimulation of long nerves involved in lower limb movement significantly reduced damage to myelin and improved motor function in a mouse model of Charcot-Marie-Tooth type 1A (CMT1A) disease, a study showed.
These benefits were associated with a reduction in the damaging accumulation of a myelin protein called peripheral myelin protein 22 (PMP22), a hallmark of CMT1A.
Myelin is the fatty, protective sheath around nerve fibers, or axons, that allows fast transmission of electrical signals between nerve cells (neurons) and between nerve and muscle cells.
The findings point to electrical nerve stimulation as a potential therapeutic approach for people with CMT1A and other conditions affecting myelin in peripheral nerves, the researchers said.
The study, “Implantable Electroceutical Approach Improves Myelination by Restoring Membrane Integrity in a Mouse Model of Peripheral Demyelinating Neuropathy,” was published in Advanced Science.
Myelin loss, called demyelination, leads to a number of conditions that affect either the central nervous system (CNS; the brain and spinal cord) or the peripheral nervous system (PNS).
Demyelination in the PNS — the network of nerves that relay motor and sensory signals back and forth between the arms and legs and the CNS — is a hallmark of CMT type 1, also known as “demyelinating CMT.”
Its most common subtype, CMT1A, is commonly caused by a duplication of the PMP22 gene. This leads to the overproduction of PMP22, a critical component of the myelin sheath, by Schwann cells, which are responsible for producing the myelin sheath outside the CNS.
PMP22’s accumulation disrupts myelin’s structure and function, leaving axons unprotected, slowing nerve cell communication, and resulting ultimately in neuronal damage.
Testing electrical nerve stimulation
Electrical nerve stimulation, or applying an electrical current directly to nerves, is gaining interest as a potential therapy for diseases associated with nerve cell damage in both the CNS and PNS.
Preclinical research suggested this approach may improve peripheral nerve growth, function, and repair, as well as Schwann cell movement.
Researchers in South Korea showed that electrical nerve stimulation promoted myelin production, or myelination, in lab-grown mouse dorsal root ganglion (DRG), a region that contains the cell bodies of sensory nerves.
The same research team has provided the first evidence that it may reduce myelin loss and improve motor function in peripheral demyelinating diseases such as CMT type 1.
The researchers used a mouse model of CMT1A. These mice carry a PMP22 mutation that leads to progressive peripheral nerve demyelination and motor decline.
The model also shows abnormalities in the distribution of PMP22 and cholesterol in the myelin sheath. Cholesterol is one of the most abundant and essential structural fatty molecules of myelin.
The researchers first identified the optimal condition of electrical stimulation by assessing the myelinating effects of 50 millivolts and several frequencies in lab-grown Schwann cells and sensory nerves from the CMT1A mouse model relative to healthy mice.
Improved myelination, more myelinated neurons
This condition was further tested in whole DRG carefully removed from these mice and grown in the lab. Electrical stimulation significantly improved myelination and increased the number of myelinated neurons, “bringing them closer to the levels observed in [healthy] DRGs,” the researchers wrote.
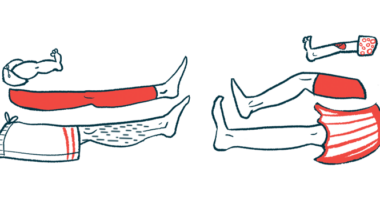
The team next evaluated the effects of this optimal electrical stimulation, delivered via flexible electrodes implanted onto the sciatic nerves of the mice. The sciatic nerves, the longest and thickest nerves in the human body, control motor and sensory functions of the legs and feet.
Mice undergoing the intervention, administered at the beginning of each week for three consecutive weeks, showed gradual, significant improvements in balance and running endurance relative to untreated mice. Treated mice also showed significantly greater improvements over time than both untreated animals and healthy mice.
Also, at the end of the three weeks of treatment, the animals’ sciatic nerves showed a significant, partial restoration of myelin sheath thickness, compactness, and integrity. The frequency of demyelinated or thinly myelinated axons was also greatly reduced, closely resembling that observed for healthy mice.
These beneficial effects were associated with a significant reduction in the distribution abnormalities of PMP22 and cholesterol in the myelin sheath, “revealing the restoration of myelin membrane integrity,” the researchers wrote.
This suggests electrical nerve stimulation may eliminate the need for lipid supplementation in patients, thereby avoiding the likely side effects of such fat-rich approaches, the researchers noted.
“This study demonstrates, for the first time, that [electrical nerve stimulation] has the potential to treat CMT disease and restore impaired myelin membrane integrity, shifting the paradigm toward practical interventions for peripheral demyelinating neuropathies [nerve-damage conditions],” the researchers said, noting their findings should “lay the groundwork for the development of electroceutical treatments for peripheral demyelinating neuropathies, which can be realized via further elucidation of the mechanism and the maturation of neuromodulation technologies.”
Electroceuticals, medical devices that provide neurostimulation for therapy, have evolved, becoming miniature, wireless, and flexible devices that can be implanted through less invasive procedures.
More studies are needed to confirm the findings in other models of “demyelinating CMT” and in older animals with greater neuronal and motor deficits, the researchers said.