CMTA awards more than $225K to develop CMT2E treatments
Project to develop therapies that can stop production of abnormal NfL protein
The Charcot-Marie-Tooth Association (CMTA) has given a $225,483 award to support the development of treatments for Charcot-Marie-Tooth disease type 2E (CMT2E).
The work is also being supported by the Muscular Dystrophy Association. The project will be led by Mario Saporta, MD, PhD, clinical neurologist and researcher at the University of Miami.
“We are thrilled to collaborate with CMTA in order to fund meaningful research that could impact many individuals living with Charcot-Marie-Tooth disease,” Sharon Hesterlee, PhD, chief research officer of the MDA, said in a press release.
Project ‘supported by the CMTA-STAR initiative since day one’
“We are very excited to continue this long-standing collaboration with the CMTA,” Saporta said. “This project has been supported by the CMTA-STAR initiative since day one and foundational work to characterize the human cellular model we are now using to validate our treatment strategy was a product of previous grants received from the CMTA.”
CMT2E is caused by mutations in the gene NEFL, which provides instructions for making a protein known as neurofilament light chain (NfL). Mutations in this gene also cause CMT type 1F.
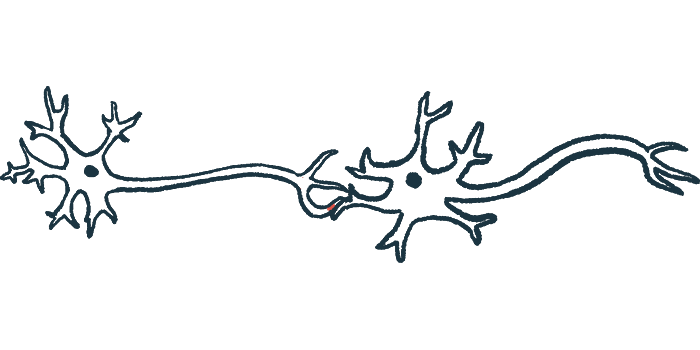
The NfL protein normally functions to help support axons, which are the long, wire-like fibers that nerves use to connect with each other. Sort of like scaffolding supporting a building, NfL proteins connect with each other to provide structural support for the axon.
Everyone inherits two copies of the NEFL gene, one from each biological parent. In people with CMT2E, only one copy of this gene carries a disease-causing mutation that produces a defective version of the NfL protein. The other gene copy is healthy, encoding a normal version of the protein.
The defective NfL protein is able to stick to healthy versions of the protein, causing both the defective and healthy proteins to form clumps. This prevents NfL from providing the needed structural support to nerve fibers, ultimately resulting in the nerve damage that drives disease symptoms in CMT2E.
The new project aims to develop therapies that can stop the production of abnormal NfL protein while still allowing the healthy version of the protein to be made so that it can give structural support to nerves. Researchers specifically hope to develop molecules called antisense oligonucleotides, or ASOs.
When the NEFL gene is “read” to produce NfL protein, the genetic code is copied from the cell’s DNA into a temporary molecule called messenger RNA (mRNA). The mRNA is then shipped to the cell’s protein-making factories called ribosomes, which use the mRNA as a template to make NfL protein.
ASOs are small pieces of nucleic acid (the building blocks of DNA and RNA) that can be designed so they stick to mRNA from a specific gene — in this case, the NEFL gene carrying the disease-causing mutation. When the ASO sticks to the mRNA, it triggers the mRNA to be destroyed. By destroying the mRNA, these therapies work to decrease the production of mutated NfL protein.
The newly funded study will test this approach in cell models. If the results are positive, then this approach could be expanded to create similar therapies targeting other types of CMT. Data gleaned from the study may also help researchers to better understand the function of NfL in nerve fibers.
“We look forward to seeing this treatment approach advance into animal models and then patients,” Saporta said.








