HDAC6 Inhibitors Restore Neuromuscular Defects in Zebrafish
Written by |
Treatment with inhibitors of the HDAC6 protein, including the new compound CKD-504, was able to restore proper connections between nerves and muscles and improve movement in zebrafish with low levels of GARS — the gene implicated in Charcot-Marie-Tooth disease type 2D, a study found.
The results suggest that HDAC6 blockade may be a promising therapeutic strategy for CMT2D and other diseases where nerve-muscle communication is impaired, the researchers suggested.
The study, “Therapeutic Potential of CKD-504, a Novel Selective Histone Deacetylase 6 Inhibitor, in a Zebrafish Model of Neuromuscular Junction Disorders,” was published in Molecules and Cells.
CMT2D is caused by mutations in the GARS gene, which provides instructions for making the GlyRS enzyme. Symptoms of CMT2D, like other CMT forms, include damage to the nerves outside the brain and spinal cord (peripheral nerves), leading to muscle weakness and wasting.
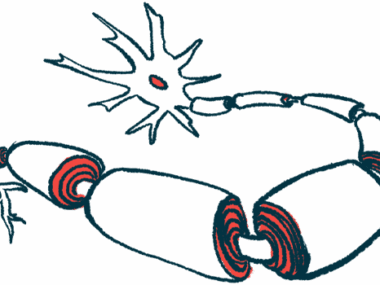
GlyRS is involved in signaling at the neuromuscular junction (NMJ), the place where nerves and muscle fibers meet to communicate, and mouse models with Gars mutations show notable NMJ malformations and nerve cell problems. Gars is the mouse form of GARS.
Targeting NMJ impairment may be a promising therapeutic strategy for CMT2D, the researchers hypothesized.
HDAC6 inhibitors have recently emerged as a potential treatment for some types of CMT, including type 1 and type 2, but their effects on NMJ function have not been established.
The research team examined whether several different HDAC6 inhibitors could restore NMJ defects in a zebrafish model of CMT.
In this model, zebrafish larvae were genetically engineered to have lower levels of the gars gene, mimicking the symptoms of CMT2D. The researchers found that the gars-lacking zebrafish had fewer NMJs than those with normal gene levels, but normal brain development overall.
The swimming velocity of the larvae over 30 minutes was assessed as a measure of motor function. Those fish with depleted gars moved significantly less and were slower than their healthy counterparts.
In an attempt to “rescue” the zebrafish with low gars levels, the team injected them with a healthy human form of the gene, which successfully reversed the NMJ and movement deficits previously observed, supporting the hypothesis that GARS is important for NMJ function, the researchers said.
In nerve fibers, microtubules are responsible for moving proteins and cell compartments to their proper place. They are formed by alpha-tubulin, which needs to undergo a type of modification called acetylation to function properly. The researchers found that the genetically modified zebrafish had increases in alpha-tubulin deacetylation, which causes microtubules to become unstable.
Previous research indicated HDAC6 interacts abnormally with GlyRS, the protein product of GARS, leading to lower acetylation of alpha-tubulin. Another study showed the HDAC6 inhibitor CKD-504 increased acetylated alpha-tubulin and eased deficits in nerve activation in human spinal cord cells with GARS mutations.
The team tested whether CKD-504, originally developed to treat Huntington’s disease, could restore the observed deficits in the zebrafish larvae. They found that the treatment effectively restored more normal NMJs and improved movement.
Other HDAC6 inhibitors — namely, tubastatin A, vorinostat, and pomiferin — were also able to repair the defects.
Vorinostat and pomiferin are broad-acting inhibitors that affect HDAC6 in addition to other proteins in the HDAC family. Both have shown efficacy against cancer (vorinostat is the first treatment approved in the U.S. for cutaneous T-cell lymphoma), but not in neuromuscular diseases. CKD-504 acts specifically on the acetylation of alpha-tubulin and has shown promise in treating neurological disorders.
The results suggest that HDAC6 inhibition, particularly with CKD-504, may be a promising therapeutic approach for CMT2D.
The therapy may be effective in other neuromuscular disorders, such as distal motor hereditary neuropathy type 5, which is also sometimes caused by GARS mutations.
“The molecular mechanisms by which GARS regulates NMJ formation and function and how HDAC6 inhibitors directly affect GARS in NMJs remain unclear,” the researchers wrote, noting that HDAC6 inhibition improves the stability of microtubules needed for proper NMJ function.
“Therefore, future studies are needed to elucidate the molecular mechanisms by which CKD-504 restores NMJ defects using more NMJ-related disease models,” they concluded.