CMT Type X May Be Risk Factor for Multiple Sclerosis, Study Suggests
Written by |
Charcot-Marie-Tooth disease type X (CMTX) may increase the risk of developing multiple sclerosis (MS), the most common central nervous system inflammatory demyelinating disease, according to data from a Greek study.
The study, “X linked Charcot-Marie-Tooth disease and multiple sclerosis: emerging evidence for an association” was published in the Journal of Neurology, Neurosurgery and Psychiatry.
CMTX is the second most common type of Charcot-Marie-Tooth, accounting for 8-15% of all cases, and is caused by a mutation located in the X chromosome.
Men, with only one X chromosome, have more severe symptoms than women, who have two (in females, one copy is often called a backup copy in case there are abnormalities in the other X chromosome).
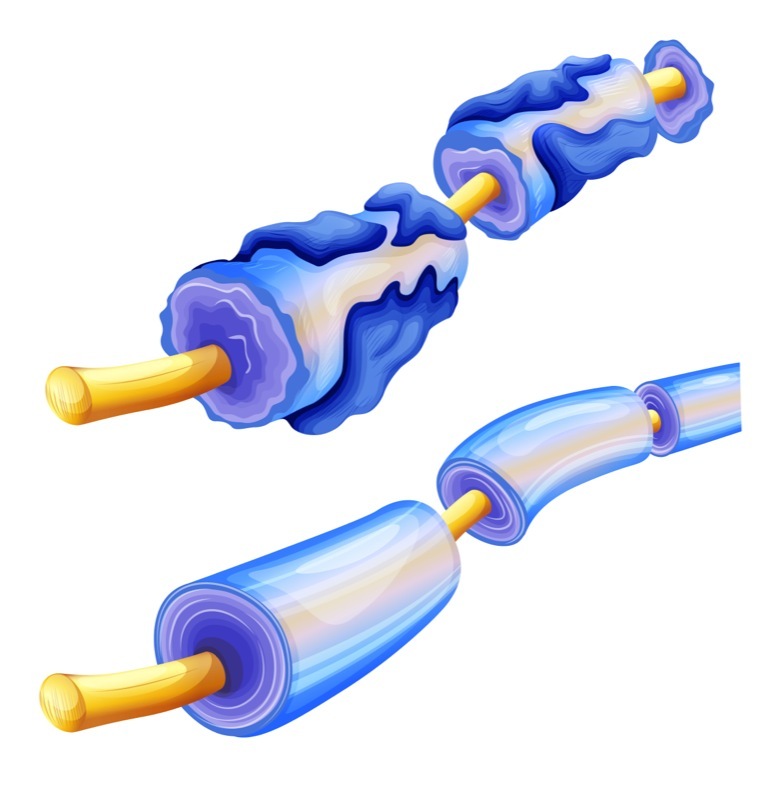
CMTX is characterized by an overly thin protective layer of myelin surrounding nerve fibers of peripheral nerve cells, those that connect the brain and spinal cord to muscles and sensory organs.
This causes progressive nerve cell degeneration, leading to muscle weakness and atrophy, and decreased sensation (touch, pain, or heat), mainly in the feet, legs, hands, and forearms.
In the last 20 years, several studies have linked CMT with multiple sclerosis, an immune-mediated neurodegenerative disorder characterized by the loss of the myelin sheath that protects nerve cells.
Among these studies, at least four cases of patients with CMTX report they also developed signs of demyelination (loss of myelin) that is compatible with a diagnosis of MS.
Researchers at the School of Medicine, National and Kapodistrian University of Athens in Greece, set out to investigate the potential link between CMTX and MS.
They measured the frequency of MS among a group of Greek patients with CMTX.
In total, their group included 70 patients with CMTX (all positive for mutations in the GJB1 gene, located on the X chromosome) and with symptoms and signs suggestive of multiple sclerosis.
All of them underwent a brain scan by magnetic resonance imaging (MRI) and, where possible, analysis of the cerebrospinal fluid (collected by a lumbar puncture) to confirm an MS diagnosis. Cerebrospinal fluid is the liquid around your brain and spinal cord.
Additionally, they included a group of 18 CMTX patients without any signs of MS and 18 age- and gender-matched healthy individuals as controls. All of them also underwent brain MRI scans.
Blood samples from two patients with CMTX and MS were also investigated for evidence of autoimmunity.
Out the 70 patients diagnosed with CMTX, three of them fulfilled the criteria for MS: two male patients, one in his 50s and the other in his 60s, and one woman, age 47.
Their brain MRIs showed signs of myelin damage (old and new) in the brain and spinal cord (the so-called T2 hyperintense lesions) and they tested positive for gadolinium, a large molecule that only enters the central nervous system when there is active inflammation.
Patients also showed impairments in their ability to walk and signs of muscle shirking (atrophy). In two of the cases, neuropsychological tests revealed impairments in verbal and visuo-spatial working memory.
The blood analysis from the two patients with CMTX and signs of MS tested negative for the presence of autoantibodies, those that trigger autoimmune disorders because they attack the body’s own tissues.
Within the group of 18 patients with CMTX but no evidence of MS symptoms, 10 of them showed signs of T2-hyperintense lesions in the corpus callosum, the bridge between the left and right sides of the brain. No such signs were found in the healthy controls.
This study “presents circumstantial evidence for an association between CMTX and an inflammatory [central nervous system] demyelinating disease fulfilling diagnostic criteria for MS, suggesting that pathogenic mutations in GJB1 may act as a rare risk factor for the development of MS,” researchers wrote.





