Certain NEFH Mutations Linked to Atypical Form of CMT

Mutations in a particular region of the neurofilament heavy chain or NEFH gene cause an atypical, more severe form of Charcot-Marie-Tooth disease, called type 2CC or CMT2CC, according to a study reporting the cases of 30 patients from eight unrelated families.
Notably, the presentation and progression of this subtype more resemble spinal muscular atrophy — a progressive disorder that mainly affects muscles closer to the center of the body — than classic CMT.
These findings provide insights on the features and genetic causes of CMT2CC, which may help in its diagnosis and in the identification of new therapeutic targets and approaches, the researchers said.
The study, “Charcot-Marie-Tooth disease type 2CC due to NEFH variants causes a progressive, non-length-dependent, motor-predominant phenotype,” was published in the Journal of Neurology, Neurosurgery and Psychiatry.
Neurofilaments, consisting of three major subunits — heavy, intermediate, and light chains — are major structural proteins of neurons and key for the growth and function of nerve cell fibers, or axons.
When axons are damaged and neurons die, neurofilaments are released into the cerebrospinal fluid (CSF) and bloodstream, and as such, they have been used as potential biomarkers of neuronal damage in several neurodegenerative conditions. Of note, the CSF is the liquid that surrounds the brain and spinal cord.
In addition, prior research suggests that neurofilaments and their subunits can accumulate and form aggregates or clumps that may affect nerve cells’ function.
Mutations in the neurofilament light chain (NEFL) gene are estimated to cause 2% of all CMT cases, including subtypes of “demyelinating CMT,” also known as CMT type 1 (CMT1), and “axonal CMT,” or CMT type 2 (CMT2).
Demyelinating CMT is characterized by progressive demyelination, or loss of myelin, which is the protective sheath around axons, while axonal CMT is identified by axonal degeneration. Both types affect the peripheral nervous system, which controls movement and sensation in the limbs.
Notably, few studies have reported mutations in the NEFH gene in people with CMT type 2CC, but no comprehensive characterization of this subtype has been conducted to date.
To address this, an international team of researchers in the U.K., France, and South Korea detailed the symptoms and progression of CMT2CC due to NEFH mutations in 33 people from eight unrelated families followed at their centers.
A total of 30 people showed disease symptoms, while three — with ages of 6, 17, and 23 — did not, and thus would be known as asymptomatic. However, two of these asymptomatic carriers of NEFH mutations already showed evidence of axonal damage on specific tests.
Symptom onset of most (73.3%) affected patients occurred in mid-adulthood, at a mean age of 31. Still, eight (26.7%) patients had disease onset during their childhood or teenage years.
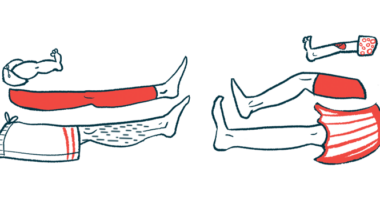
CMT2CC was mostly associated with lower limb- and motor-predominant symptoms. The upper limbs were mildly affected, with sensory symptoms were reported by only three patients.
For 70% of patients, muscle weakness of the proximal leg muscles, or those located more closely to the body’s center, became evident early in the disease course, after a mean of 4.4 years following symptom onset.
This early muscle weakness usually affected patients’ ability to climb stairs, walk uphill, or stand from a sitting position. Notably, the disease progressed rapidly — unlike other CMT subtypes — as half (53%) of the patients needed to use a wheelchair or a mobility scooter after a mean of 24.1 years following symptom onset.
Also, 40% of patients had evidence of early muscle weakness in the ankles, “a feature which is observed in only a handful of CMT subtypes,” the researchers wrote.
Both motor and sensory responses were universally reduced or absent in the lower limbs, but not in the upper limbs, where impaired motor responses were detected only in two patients older than 65.
Additional tests confirmed that the disease was associated with non-length-dependent axonal damage in most of the patients. This means that, in contrast to typical axonal CMT, CMT2CC does not affect first the longer axons that control movement and sensation in the periphery of the body — such as the feet, lower legs, hands, and forearms.
Nerve damage severity varied between patients, regardless of their ages. Two families showed disease variability between members, with successive generations of affected individuals showing an earlier symptom onset and/or a more severe disease.
Genetic analysis revealed six likely disease-causing frameshift mutations at the end of the NEFH gene, all resulting in the production of a longer-than-normal protein with 42–47 additional amino acids (the building blocks of proteins).
Frameshift mutations shift the way the DNA sequence is read following the mutation, resulting in an incorrect amino acid sequence that can be either longer or shorter than the normal protein.
All mutations were inherited in a dominant manner, meaning that a child only had to inherit one mutated copy of the NEFH gene to develop the disease.
Also, these NEFH mutations were identified in eight initial patients — the first identified patients from each family — among 2,494 CMT patients screened at the three study centers since 2016, “confirming the rarity of NEFH variants in CMT,” the team wrote.
These findings highlight “the unusual [features] of CMT2CC, which is more akin to spinal muscular atrophy rather than classic CMT,” and “progresses faster than expected for classical CMT with at least half of the patients losing independent [walking abilities] by the seventh decade of life,” the researchers wrote.
This comprehensive characterization of CMT2CC may “enable more informative discussions on the natural history of the disease and will aid in NEFH variant interpretation in the context of the disease’s unique molecular genetics,” the researchers wrote.
Also, the unique link between frameshift mutations at the end of the NEFH gene and this subtype “may open potential avenues for the development of rational genetic therapies,” the team concluded.