PMP22 Defects May Be Link Between CMT1A and MS, Case Report Says

Defects in PMP22, the protein involved in Charcot-Marie-Tooth disease type 1A (CMT1A), might play a role in the loss of myelin — the fatty substance that protects nerve fibers — associated with multiple sclerosis (MS), according to a case report.
The case report study, “A special association between Charcot-Marie-Tooth type 1A disease and relapsing remitting multiple sclerosis,” was published in Multiple Sclerosis and Related Disorders.
Charcot-Marie-Tooth (CMT) is the most common heritable disease that affects the peripheral nervous system — the network of nerves responsible for controlling movement and sensation in the limbs. The disease can be caused by different genetic mutations and manifest at various ages, depending on its type and subtype.
In certain subtypes of CMT, there have been cases of patients whose symptoms or type of brain lesions suggested a direct involvement of the central nervous system (CNS, composed of the brain, brainstem, and cerebellum).
“Also, data from literature reported the association between CMT1A/1B and MS, supported by genetic studies and clinical investigations showing a possible [loss of myelin] process,” the authors wrote.
In this case report study, physicians described the case of a young woman who had CMT1A and MS, supporting the idea that the conditions might have a common mechanism.
When she was admitted to the rehabilitation department, the 21-year-old had a history of gait impairments lasting approximately six years, and a history of MS over the last three years. She also had a family history of peripheral neuropathy and claimed she had pes cavus (high foot arch) — a foot deformity associated with CMT — since childhood.
She also had a history of acute psychosis and mental health impairments that worsened after she received several doses of intravenous methylprednisolone to treat her MS relapses. After that she started treatment with the immunomodulatory agent glatiramer acetate and later was started on fampridine.
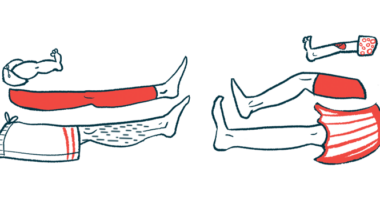
During physical examination, she showed gait impairment, mild peripheral atrophy in her arms and legs, pes cavus, hammer toes, mild loss of sensation in her legs and urinary incontinence.
Electrophysiological (the study of how electrical signals are transmitted through nerves in the body) analyses confirmed she had an inherited form of peripheral neuropathy, whereas brain magnetic resonance imaging (MRI) revealed she had several lesions in different regions of the brain that suggested the presence of a demyelinating disease.
Genetic tests performed afterward confirmed she had CMT1A caused by a duplication of the PMP22 gene.
“Our patient is one of the rare cases with CMT1A that developed a demyelinating illness fulfilling the diagnostic criteria for MS. The increasing number of cases with CMT and MS may point to the relationship between the two diseases, [possibly resulting from duplications on the PMP22 gene],” they stated.
“PMP22, the target protein in CMT1A [and] a component of myelin, [is very similar] with other CNS proteins. [Therefore,] the PMP22 gene might be relevant to a common pathway of the demyelinating process.
“In conclusion, although the simultaneous existence of CMT1A and MS in our patient could be coincidental, we suggest that inherited peripheral demyelination may trigger an autoimmune reaction against CNS myelin.”