Technique Reveals Unique Protein Structure of PMP22
Written by |
Researchers at the University of Michigan and Vanderbilt University have found that mutant PMP22 proteins pair to form a unique, stabilized complex called a dimer.
The discovery, which was made using an advanced protein analysis technique, provides new insight into PMP22’s role in Charcot-Marie-Tooth (CMT) disease and may have potential as a therapeutic target.
The study, “Ion Mobility Mass Spectrometry Reveals the Role of Peripheral Myelin Protein Dimers in Peripheral Neuropathy,” was published in the journal Proceedings of the National Academy of Sciences.
Both CMT type 1A and some forms of CMT type 3 (also called Dejerine-Sottas syndrome) are caused by mutations in the PMP22 gene that result in dysfunctional PMP22 protein. PMP22 is a component of myelin, a protective coating wrapped around nerves that enables the transmission of signals in the nervous system.
Although mutant PMP22 is known to be involved in CMT, the precise relationship between the protein and the disease is not well-understood. This study explored PMP22’s protein folding — the formation of a protein into its three-dimensional structure, which is critical to its function.
Generally, when proteins are misfolded, they are either degraded or clumped together in a way that prevents normal function.
Charles Sanders, PhD, an associate dean for research at Vanderbilt University, Nashville, Tennessee, has studied PMP22 for more than two decades. In that time, he has collaborated with Melanie Ohi, PhD, an associate professor at the University of Michigan and Sanders’ former colleague at Vanderbilt, on research exploring the normal function of PMP22.
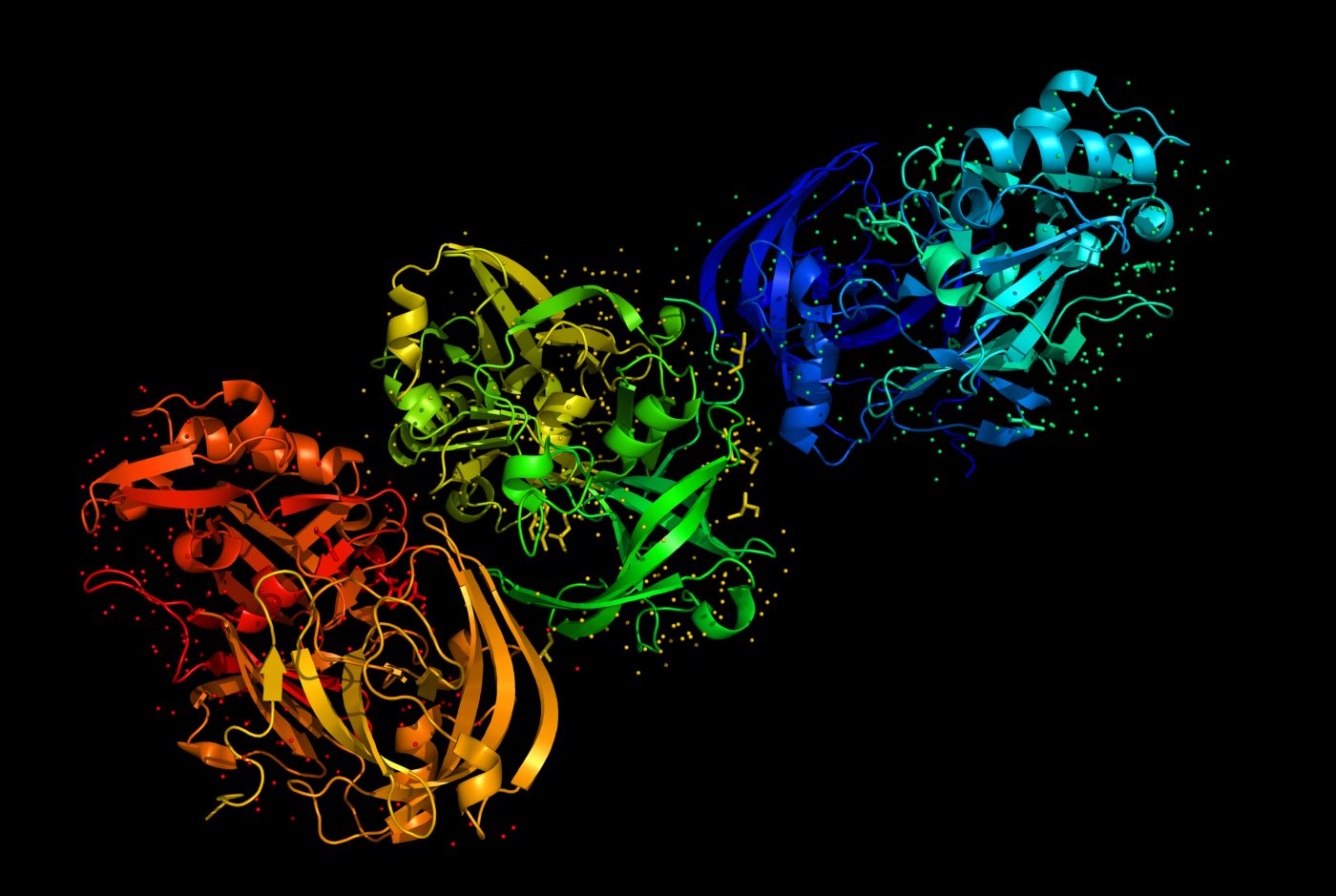
Ohi began collaborating with Brandon Ruotolo, PhD, an expert in the ion mobility-mass spectrometry (IM-MS) technique used in the study, to further investigate the structure of PMP22 and what role its structure plays in the protein’s function.
“We were able to see what we called myelin-like assemblies that allowed us to get some idea of what this protein might actually be doing … Our goal was to get a high-resolution structure, which is really hard because this is a really small protein,” Ohi said in a press release.
IM-MS requires converting the proteins into charged droplets, using a technique called nano-electrospray ionization. When the solution carrying the protein dries, they are drawn into a vacuum environment inside the mass spectrometer, where, after a series of steps to separate charged particles, the scientists are able to view PMP22 structure.
When analyzing mutant PMP22 structure, the team observed that the protein is unstable and does not fold correctly. But, rather than being degraded, it forms misfolded dimers. Notably, dimers are made of two single units called monomers.
“Because it’s stable, it’s not going to re-form into monomeric protein that is then going to give you normal myelin sheath production,” said Ruotolo, the study’s lead investigator and professor of chemistry at the University of Michigan.
“We still don’t know exactly what it then does to cause these diseases,” Sanders added, “but it’s an interesting and unusual observation that makes these diseases different from all of the other protein-folding diseases.”
Sanders emphasized the potential of IM-MS as a means of advancing both disease research and treatment development. “You could imagine eventually extending this to drug discovery, using this basic method as an assay for finding compounds that correct these defects,” he said.





