Being Heavy Does Not Worsen Nerve Function in Charcot–Marie–Tooth Disease type 1A, Study Suggests
Written by |
Being overweight does not worsen nerve function in people with Charcot–Marie–Tooth Disease type 1A (CMT1A), but it may lead to more pain and less muscle strength in lower extremities, a study reports.
Researchers published the study in the Journal of Clinical Neurophysiology. Its title is “Charcot–Marie–Tooth Disease Type 1A: Influence of Body Mass Index on Nerve Conduction Studies and on the Charcot–Marie–Tooth Examination Score.”
The cause of CMT1A is a genetic defect — specifically, duplication of the gene that produces peripheral myelin protein 22, or PMP 22. Loss of this protein, which helps protects nerve cells, is a hallmark of a neurodegenerative condition like CMT.
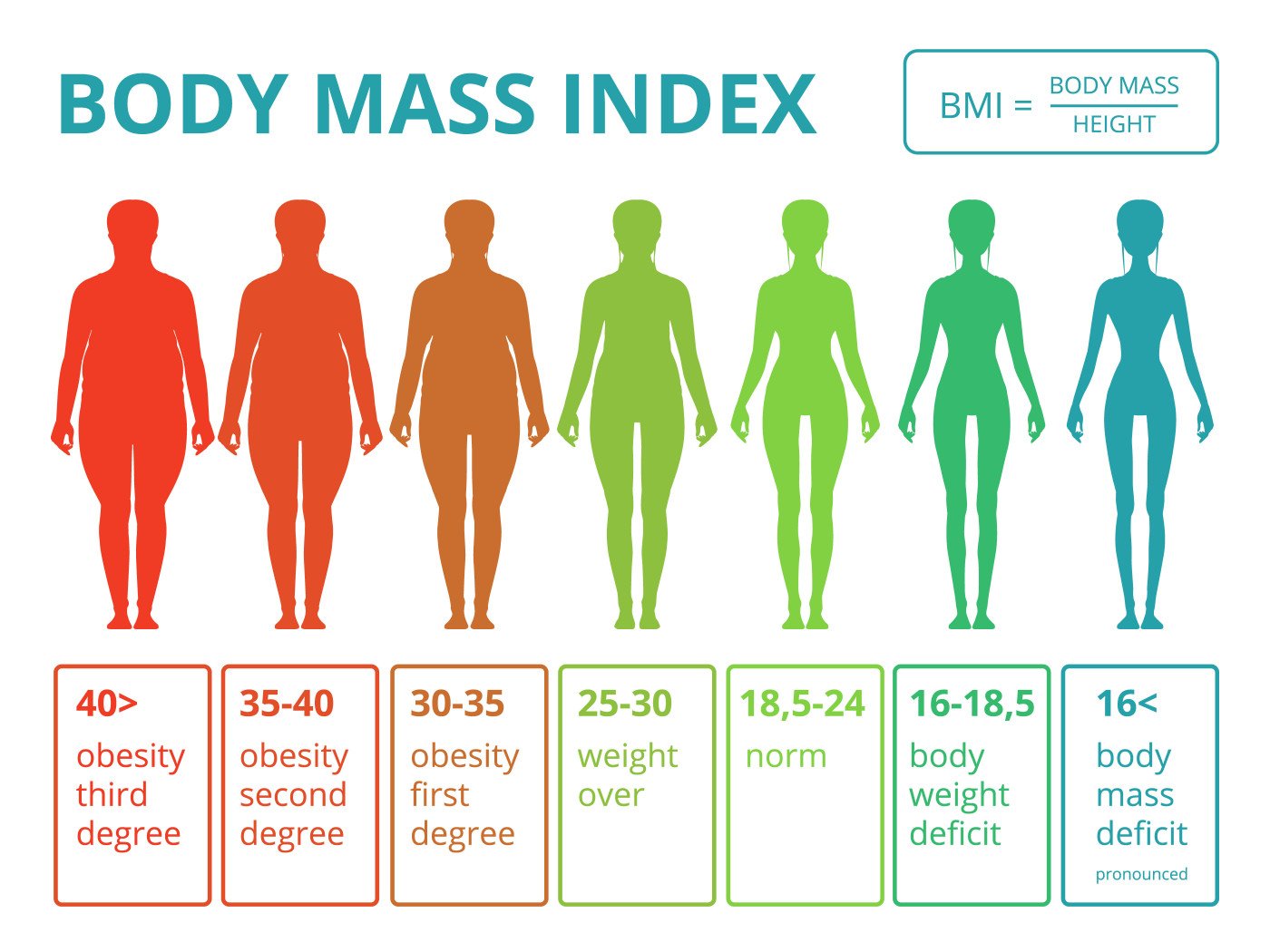
Studies have suggested that Type 2 diabetes can worsen CMT1A outcomes. A common characteristic of Type 2 patients is a high body mass index, or BMI, a score that takes into account a person’s fat level, height and weight.
But there has been limited information on “whether body mass index affects electrophysiological [nerve-signal transmission] or clinical [disease] data in those with CMT1A,” researchers at the University of Iowa’s Carver College of Medicine wrote.
They wanted to know if being overweight would affect Charcot–Marie–Tooth severity scores and patients’ ability to transmit nerve signals — what scientists call nerve conduction.
Researchers combed through CMT1A patients’ records in a University of Iowa patient database. They looked at patients’ body mass index and electrodiagnostic test scores, which measure nerve conduction. They also recorded patients’ sex and the ages at which they received electrodiagnostic tests.
The patients included 51 men and 50 women whose average age was 41.
Normal BMI is 19 to 25. The average BMI of the Iowa CMT1A patients was 28. Thirty-two were obese — that is, they had a mean BMI of 36. The BMI of the 69 non-obese patients was 23.
The patients with a higher BMI were eight years older than those with a lower BMI – 45 versus 37.
After adjusting for patients’ age, the researchers found that a higher BMI had no effect on ulnar motor nerve functioning or nerve conduction scores. The ulnar motor nerve controls muscles in the forearm and hand.
The team said the results confirmed their hypothesis that increased production of PMP 22 plays a more important role than body mass index in “the neurophysiological patterns of CMT1A.”
Further analysis suggested a link between higher BMI, worse lower extremity pain and less lower extremity muscle strength.
“Whether the loss of lower extremity pinprick sensation and motor strength results in a higher BMI or if higher BMI results in these signs” requires further clarification, the researchers concluded.





