Reduced Physical Activity Has Negative Effect on Children with CMT, Study Suggests

Lack of physical activity among children and adolescents with Charcot-Marie-Tooth (CMT) disease has a long-term negative effect on their physical function.
The study with that finding, available in the BioRxiv platform, is titled “Physical activity in children and adolescents with Charcot-Marie-Tooth disease: a cross-sectional case-controlled study.”
CMT is characterized by motor and sensory dysfunction and progressive muscle weakness that limits physical activities such as walking, running and jumping. Compared with unaffected adults, patients with CMT are less physically active.
It is known that reduced physical activity in the general population increases health-related illnesses, and this negative outcome likely adds to the effects of nerve disorders.
A group of researchers conducted a study to estimate the level of physical activity in pediatric CMT and explored its relation with disease progression.
The team collected data from 50 children with CMT, mean age 12.5 years, with various disease subtypes attending two Australian pediatric neuromuscular centers and 50 age- and sex-matched healthy controls.
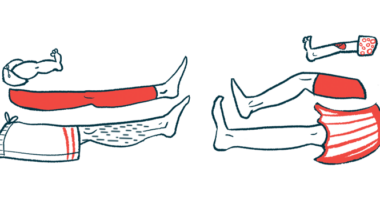
The participants answered the physical activity questionnaire – child (PAQ-C) to assess physical activity, while the Walk-12 questionnaire and the 6-minute walk test (6MWT) were used to measure their ambulatory capacity.
The Walk-12 questionnaire is a self-reported survey that assesses children’s experience and perception of the limitations of their disease as it relates to gait and gait-related activities. The 6MWT measures the maximum distance an individual can walk for six minutes on a hard, flat surface. The person walks at their own pace and can stop and rest as many times as needed.
According to the questionnaire answers, CMT children were less active. Researchers estimated that the CMT group spent an average of 283.6 minutes per week on physical activities, whereas the estimate was 318 minutes for the control group.
CMT participants who did not wear walking-aid devices walked a significantly shorter distance in the 6MWT compared to the matched controls — 485.1 meters vs. 639.8 meters (530 yards vs. 700 yards), respectively.
Between 50 to 75% percent of CMT participants reported that their disease somewhat affected their gate-related activities, and more than 30 percent reported moderate or greater effects on running, ascent/descent stairs, walking distance and speed, as well as increased concentration required for walking.
Researchers found a strong correlation between the level of physical activity and the distance participants walked in the ambulatory capacity test.
There also was an inverse correlation between physical activity and the severity degree of CMT, meaning that children who are more active present a milder disease and a greater capacity to perform physical functions, hence decreasing sedentary activity time.
The researchers advocate that “healthcare clinicians, researchers and funding agencies ought to engage with and promote opportunities for children with CMT to be more physically active.”
“Further research is required to determine whether facilitating greater physical activity may slow disease progression and improve physical function in the everyday lives of children and adolescents with CMT,” the study concluded.