Rare mutation drives woman’s unusual CMT symptoms: Report
Case shows need for understanding genetic biology of disease, researchers say
Written by |

A novel mutation in the MPZ gene was behind an unusual case of Charcot-Marie-Tooth disease (CMT), according to a research report.
Understanding the underlying genetic biology of CMT, especially when the disease presents in unexpected ways, will be essential for developing targeted treatments, researchers said in the study, “Novel Dominant Splicing Variant in MPZ Associated With Unusual Charcot–Marie–Tooth Disease,” published in the Journal of the Peripheral Nervous System.
CMT encompasses a group of genetic disorders characterized by damage to peripheral nerves, the nerves that extend outside the brain and spinal cord to the body and help control movement and sensation. The MPZ gene provides instructions for making a protein that plays a crucial role in the health of peripheral nerves. It’s critical for the formation of an insulating sheath called myelin, and mutations in it can cause several different types of CMT as well as other neurological disorders.
Scientists in France reported the case of a 47-year-old woman who sought medical attention due to persistent balance problems while walking. Despite her balance issues, she had no signs of muscle weakness, and an MRI of her brain showed no abnormalities. Clinical workup did, however, reveal loss of sensation in the feet, no reflexes in the Achilles tendon, and difficulty chewing and speaking. The researchers noted that these symptoms are not typical of CMT, which made diagnostic workup challenging.
Doctors turn to genetic testing to find symptoms’ cause
The clinicians initially thought the woman had chronic inflammatory demyelinating polyradiculoneuropathy (an autoimmune disorder that attacks the myelin sheath), but plasma exchange — a process in which a machine separates the liquid part of blood from the blood cells, which are then mixed with a liquid and returned to the body — did little to improve her condition, so she was managed with supportive care including physical therapy and speech therapy. In an effort to find alternative explanations, genetic testing was conducted.
The woman was found to carry a never-before-reported mutation in the MPZ gene, dubbed c.234+1G>C. “Pathogenic variants in the MPZ gene have been associated” with diseases including CMT, the researchers wrote. Through tests in cell models, they determined that it was a splicing mutation.
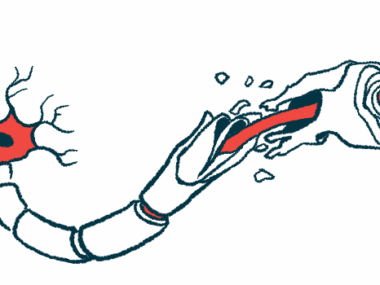
Within a cell’s DNA, the MPZ gene is comprised of sections that provide instructions to make a protein, called exons, which are interspersed with non-coding sections called introns. When the gene is read to produce protein, the entire sequence is copied into a temporary molecule called messenger RNA. The RNA then undergoes a process called splicing, where the introns are removed and the exons strung together to form a mature sequence that can be used to make protein.
The researchers found that the woman’s mutation results in the omission of one of the exons during splicing. As a result, the other exons can’t be strung together correctly, so peripheral nerve cells are unable to produce the protein needed to maintain their health. The scientists noted that splicing mutations in the MPZ gene have rarely been reported. Understanding how different mutations in this gene lead to different clinical manifestations will be important for developing treatments for people with these mutations, they said.
“Although no specific treatments are currently available for MPZ-related neuropathies [nerve diseases], proving an accurate genetic etiology [cause] to patients is essential as emerging therapies are being experimented with in this context,” the scientists wrote.