Pregnancy Can Worsen CMT Symptoms With Outcomes Unaffected, Italian Study Finds

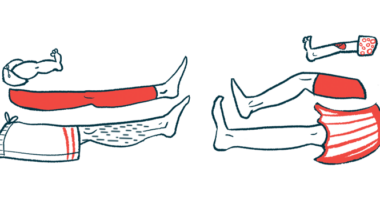
Charcot-Marie-Tooth disease (CMT) does not significantly affect the outcomes of pregnancies but a pregnancy can cause CMT symptoms to worsen, according to a study in Italy, which also recommends that expectant mothers with CMT be carefully monitored.
While outcomes such as miscarriage and newborn health were similar between women with CMT and those without the disease, researchers noticed higher rates of certain complications, such as early deliveries among those with CMT.
The study, “Pregnancy in Charcot-Marie-Tooth disease,” was published in the journal Neurology.
Although higher rates of complications and the worsening of CMT symptoms during pregnancy have been described before, no large and systematic study has addressed the issue.
Scientists from the Italian CMT Network and universities across Italy conducted a large case-control study among women with CMT registered in the Italian CMT Registry. They compiled and analyzed information on rates of pregnancy and delivery complications, newborn health, and CMT progression during pregnancy.
“The last issue might be particularly important in patients with CMT1A,” the researchers wrote, as the rising levels of progesterone during pregnancy increase expression of the PMP22 gene, an extra copy of which causes this subtype.
The investigators collected information on 139 CMT patients and 31 age-matched controls. Because the control sample was small, researchers also examined other reference populations available from National Health System data and in the scientific literature.
While more CMT patients than controls did not get pregnant, with most pointing to CMT as a contributor to the decision not to bear children, the overall rate of pregnancy per woman was similar in both groups and in the reference population.
A total of 86 women with CMT and 24 controls had detailed information about pregnancy. In CMT patients, there were 193 pregnancies, 157 deliveries with 163 newborns, and six sets of twins; in controls, there were 59 pregnancies and 46 deliveries, with one set of twins.
Approximately half of the pregnant women with CMT had CMT1A, and accounted for 109 pregnancies. The other most frequent CMT subtypes were CMT1B (seven women and 19 pregnancies), CMT2A (six patients, 12 pregnancies), CMTX1 (five patients, 10 pregnancies), CMT2I/J (four patients, seven pregnancies), and CMT2F (two patients, four pregnancies).
Women with CMT and controls showed no significant differences in terms of delivery rates (81% vs. 78%), miscarriages (11.4% vs. 15.3%), voluntary abortion (7.3% vs 6.8%), and caesarian section (emergency and planned).
Newborn weight and health did not differ between women with CMT, controls, or the broader reference population.
The greatest differences occurred in the rates of placenta previa (wherein the placenta partially or totally covers the mother’s cervix; 1.6% in patients vs. 0.4% in the reference population); abnormal fetal positions, which can complicate delivery (8.4% vs. 4.5%); and pre-term deliveries (20.3% vs. 6.9%), most of which occurred in weeks 34 to 36.
Although the investigators expected CMT symptoms to worsen primarily in women with CMT1A, they saw disease status worsen in 18 pregnancies among 14 women of diverse CMT subtypes. Eight of the 44 women with CMT1A experienced such worsening, as did two out of six with CMT2A, one of seven with CMT1B, both sole patients with CMT2E and CMT2F, and one woman with an unknown subtype.
Ten of 14 women had more than one pregnancy and, of those, four experienced disease progression in multiple pregnancies. Three women’s symptoms worsened in two out of three pregnancies, and one woman reported worsening symptoms in both of her pregnancies. The remaining six women reported worsening symptoms in only one pregnancy.
Women reported not recovering from pregnancy-related disease progression in 14 out of 18 pregnancies. Some recovery was reported in two cases with a good recovery in one and full recovery in the other.
From among these patients, the researchers saw no significant difference between women with CMT1A and those without.
The researchers cautioned that due to the study’s retrospective nature, they were unable to match all the data they collected with patient medical records, which could cause some associations to be overlooked. Nonetheless, this study was the largest to have analyzed the relationship between pregnancy and CMT to date.