New Mutations in SLC12A6 Gene Tied to Several CMT Subtypes
Researchers in Japan analyzed genetic data from CMT patients after cases of peripheral neuropathy were seen in China and Germany
Newly identified mutations in the SLC12A6 gene associated with several subtypes of Charcot-Marie-Tooth (CMT) disease have been found, according to a study in Japan. The mutations also affected the central nervous system (brain and spinal cord).
The findings call for the need to screen for mutations in the SLC12A6 gene in CMT patients, “particularly those with central nervous system lesions, such as cognitive impairment and epilepsy, regardless of the CMT subtype,” the researchers wrote.
The study “Novel heterozygous variants of SLC12A6 in Japanese families with Charcot–Marie–Tooth disease” was published in the Annals of Clinical and Translational Neurology.
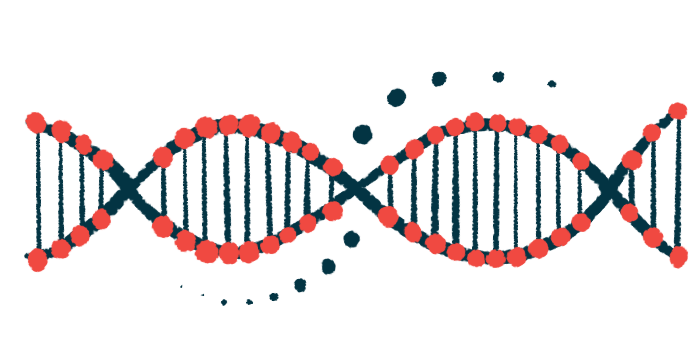
CMT is a group of inherited diseases caused by mutations in genes that impair the function of peripheral nerves, those that send sensory and motor information from the brain and spinal cord to the rest of the body.
While the most common disease-causing genetic alteration is a duplication of the PMP22 gene, more than 100 different genes have been associated with CMT and related diseases.
Mutations in the SLC12A6 gene have been linked with severe damage to peripheral nerves – a condition called peripheral neuropathy – in recent reports in China and Germany. The SLC12A6 gene contains the instructions for making a transporter protein that allows potassium and chlorine passage across the cell membrane.
Researchers in Japan analyzed genetic data from CMT patients in Japan to see if SLC12A6 mutations were also present.
In total, they analyzed DNA samples from 2,598 patients across Japan diagnosed with CMT between 2007 and 2021. They were referred for genetic analysis after showing clinical signs of peripheral neuropathy. All were negative for the PMP22 gene mutation.
In seven unrelated families, the researchers identified SLC12A6 heterozygous mutations, meaning a mutation in one gene copy. Our cells have two copies of each gene, inherited from each parent.
One mutation (p.Arg207His) had been reported previously. Three — p.Glu289Lys, p.Phe578del, p.Thr679Ser — were unknown. Two additional mutations (p.Thr580Lys and p.Ser647Pro) were classified as having uncertain significance. All five new mutations were predicted to cause disease.
The symptoms in these patients were diverse and spanned different CMT subtypes, including demyelinating (CMT type 1), axonal (CMT type 2), or intermediate forms of the disorder. Demyelination is the loss of myelin, the protective layer of nerve fibers that helps them send electrical signals efficiently.
In several patients, the central nervous system (CNS) was also affected. An intellectual disability was seen in three patients (42.9%). Another patient, a 26-year-old woman, developed epilepsy when she turned 12. MRI scans of her brain showed shrinkage (atrophy) in certain regions.
“Our findings broaden the clinical spectrum of SLC12A6 heterozygous variants, manifesting with motor and sensory polyneuropathies and CNS dysfunctions. In the clinic, it is recommended to pay more attention to CNS lesions, particularly in patients showing cognitive impairment and epilepsy,” the researchers said.