Functional Loss in CMT1A Patients May Cause Brain to Reorganize, Study Indicates
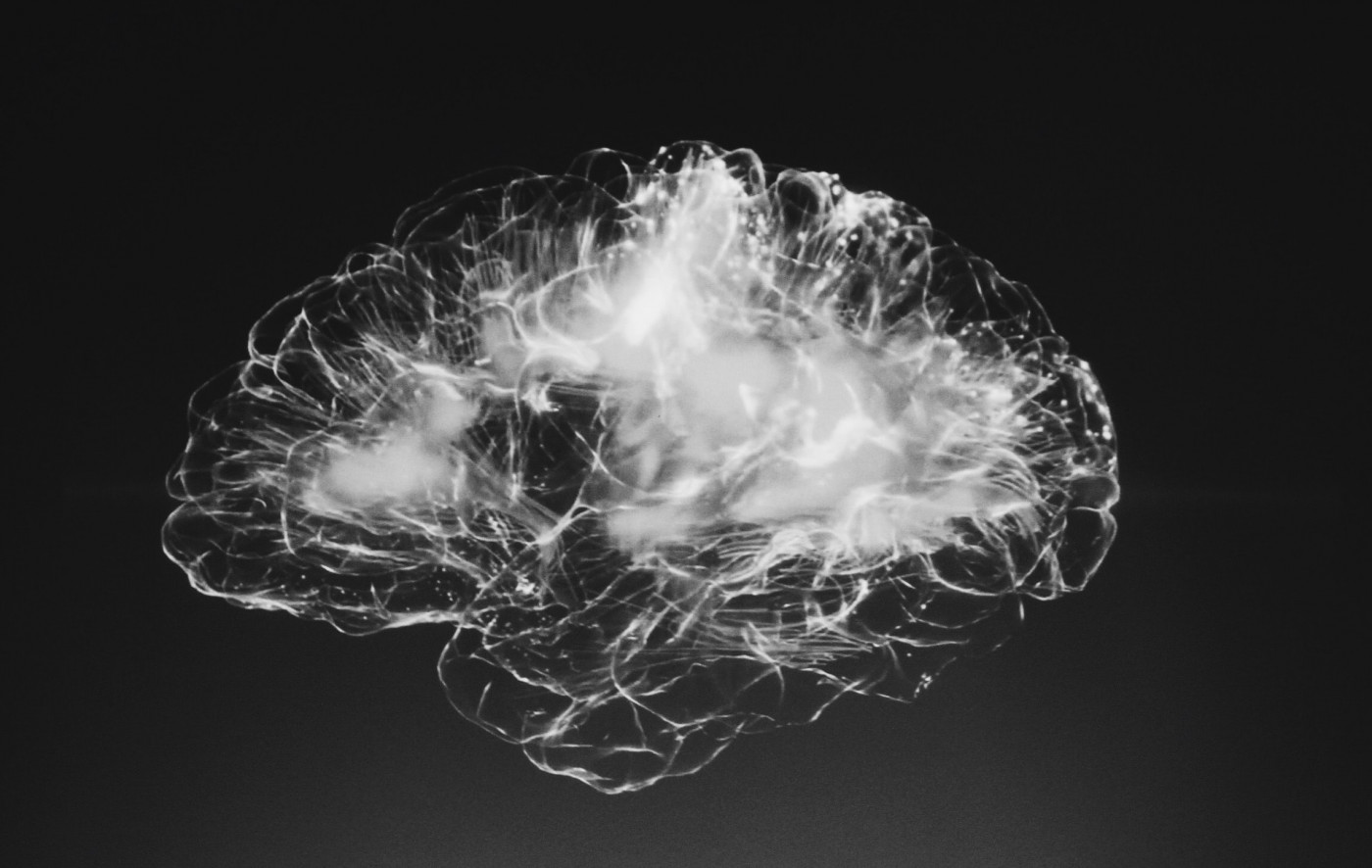
Patients with Charcot Marie Tooth Type 1A (CMT1A) disease appear to experience a structural reorganization in their brains, particularly in a region associated with movement and balance called the cerebellum, a recent study found.
These alterations, researchers suggest, may be a biological mechanism used to compensate for disease-associated changes in the peripheral nervous system — the part of the nervous system that is affected by Charcot Marie Tooth.
The study, “Brain Plasticity in Charcot-Marie-Tooth Type 1A Patients? A Combined Structural and Diffusion MRI Study,” was published in Frontiers in Neurology.
While CMT1A is a disease of the peripheral nervous system, meaning it affects the nerves relaying information between the brain and other regions in the body, the involvement of the central nervous system — consisting of the brain and spinal cord — has been revealed in previous studies.
The brain has the ability to reroute connections between its regions in response to the environment. This feature, called brain plasticity, helps the brain develop through to adulthood and allows for compensatory mechanisms in response to disease.
Researchers at the University Federico II and National Research Council, in Italy, now sought to determine if there are any changes in brain structure or evidence of plasticity correlated with functional losses in CMT1A patients.
The study included 20 CMT1A patients (mean age 34.5 years), and 20 healthy subjects comparable to patients in terms of age and sex, enrolled from 2017 to 2019.
In addition to physical examinations to assess their movement and sensory functions, participants underwent MRI exams to collect brain information.
The researchers particularly used volumetric magnetic resonance imaging (vMRI) and diffusion tensor imaging (DTI) to image the brain. vMRI is an imaging method in which internal body structures can be visualized in 3D; then 3D units called voxels are counted to measure the volume of key brain structures.
DTI is an imaging method used to visualize and measure white matter tracts (nerve fibers) in the brain. White matter tracts are responsible for carrying signals between different brain regions.
The analysis revealed that the volume of gray matter — regions containing mostly nerve cell bodies — was increased in some areas of the brain in CMT1A patients, including in the cerebellum, hippocampus, and parahippocampus.
The cerebellum is a region of the brain associated with movement and balance, whereas the hippocampus is associated with forming memory and spatial learning. Parahippocampal areas are associated with memory retrieval. No white matter differences were found in these regions.
Notably, some of the increased cerebellar grey matter volume was associated with a decreased ulnar action potential, which is involved in the movement of the wrist and fingers.
A positive correlation also was found between cerebellar volume and the neurophysiological component of the CMT Neuropathy score (CMTNS), an objective index of peripheral axonal nerve damage leading to impaired sensory function.
No significant correlations were found between gray matter density and the remaining clinical and electrophysiological functional impairment measures in CMT1A patients.
“Our data show evidence of structural reorganization in the brain of CMT1A patients, mostly involving the anterior cerebellum and possibly reflecting compensatory mechanisms in response to peripheral nerve pathology,” the scientists wrote.