mTORC1 Overactivation Linked to CMT4B Myelin Defects, Early Study Shows
Written by |
Mutations that cause Charcot-Marie-Tooth disease type 4B (CMT4B) lead to an increase in the activity of a protein called mTORC1 that is responsible for the problems with myelin that characterize the disease, a study found.
The findings suggest that mTORC1 may be a viable therapeutic target in CMT4B, the researchers said.
The study, “Rab35-regulated lipid turnover by myotubularins represses mTORC1 activity and controls myelin growth,” was published in Nature Communications.
A rare type of the disease, CMT4B is caused by mutations in the genes that encode for the MTMR2, MTMR5, and MTMR13 proteins. CMT4B-causing mutations render these proteins non-functional or entirely absent.
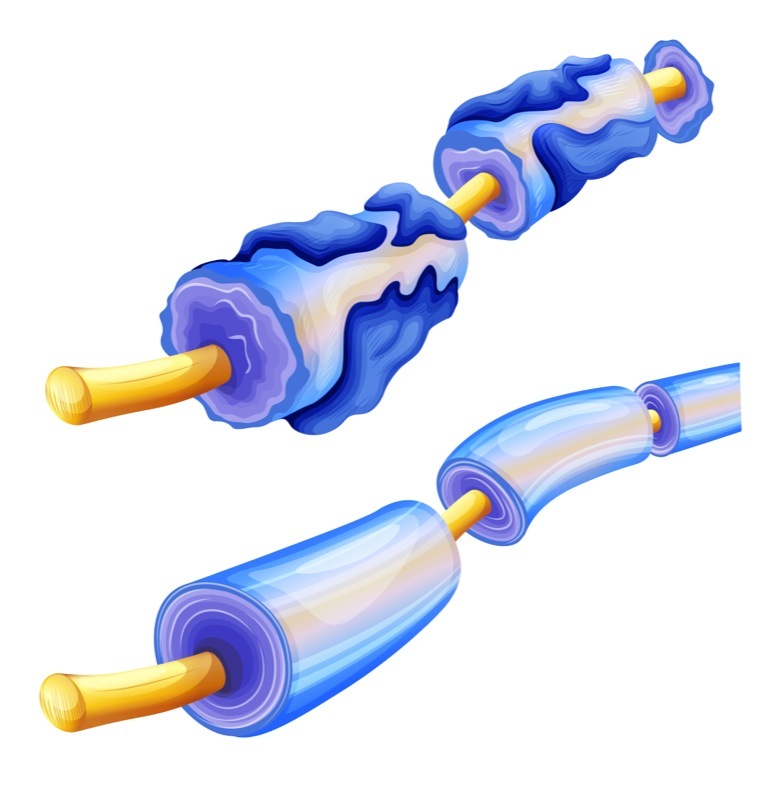
It is known that MTMRs are important for regulating certain kinds of lipids, or fat molecules, in cells. But it is not clear exactly how MTMR defects lead to the hallmark neurological feature of CMT4B, namely the excess production of myelin, which is the insulating layer or “sheath” around neurons (nerve cells) that helps them more efficiently send electric signals.
Initially, the researchers were studying another protein, called Rab35. This protein had been found to act primarily by helping other proteins get to the right parts of cells. However, exactly which proteins Rab35 usually interacts with was unclear.
Through an unbiased screen, the researchers found that Rab35 could bind to MTMR13 and MTMR5. Although it did not bind MTMR2 directly, MTMR13 and MTMR2 can bind to each other. The scientists therefore demonstrated that Rab35 could associate with MTMR2 through binding to MTMR13. Further experiments indicated that Rab35 helped regulate where within cells these MTMRs were located.
Given that impaired MTMRs lead to problems with myelin, the researchers then tested whether the activity of Rab35 was important for proper myelin formation. They generated mice that lacked Rab35 in myelin-producing Schwann cells found in the peripheral nervous system.
These mice’s neurons had areas of myelin overproduction and myelin out-folding, or improper folding — characteristic myelin defects of CMT4B.
Previous research had shown that the protein mTORC1, when overactive, could lead to similar myelin defects. Notably, mTORC1 is known to be regulated by some of the same lipids that MTMRs regulate.
Thus, the researchers hypothesized that Rab35 could — through the MTMRs it recruits — help limit the activity of mTORC1. This would explain the overproduction of myelin observed upon a lack of Rab35; functionally, the lack of Rab35 would be “cutting the brakes” on mTORC1, leading to its overactivation and subsequent myelin production.
Subsequent experiments supported this hypothesis. For instance, when the researchers decreased the activity of Rab35 or its associated MTMRs, mTORC1 activity decreased. Additional experiments suggested that this was a direct result of changes in the lipids regulated by MTMRs.
“These data suggest that Rab35 and its associated MTMRs may regulate mTORC1 activity,” the researchers wrote.
If MTMR dysfunction (as seen in CMT4B) leads to myelin defects by affecting mTORC1, then blocking the activity of mTORC1 could be a therapeutic strategy for CMT4B, the team hypothesized.
That led the researchers to investigate rapamycin, a medication approved by the U.S. Food and Drug Administration for several uses, including reducing immune system activity during organ transplants and treating certain types of cancer. This medication — which is well-studied in humans — works by blocking mTORC1.
Rapamycin was tested to determine whether it could prevent abnormal myelin production caused by a lack of Rab35. In both cells in dishes and living mice, this treatment significantly reduced abnormal myelin production, the team found.
Collectively, these data suggest that modulating mTORC1 activity — whether via rapamycin or other pharmacological strategies — may represent a viable therapeutic strategy in CMT4B.
Of note, this study was done using cells in dishes and in mice. Further research will be needed to see whether the same mechanisms are at play in human disease.
“Our work has led to the discovery of a new molecular mechanism in a particularly severe form of inherited neuropathy that is highly clinically relevant and that we now want to explore in greater depth,” Volker Haucke, PhD, a professor at Freie Universität Berlin in Germany and a study co-author, said in a press release.