Study Explores Common, Targetable Hallmark of CMT2 Subtypes
Written by |
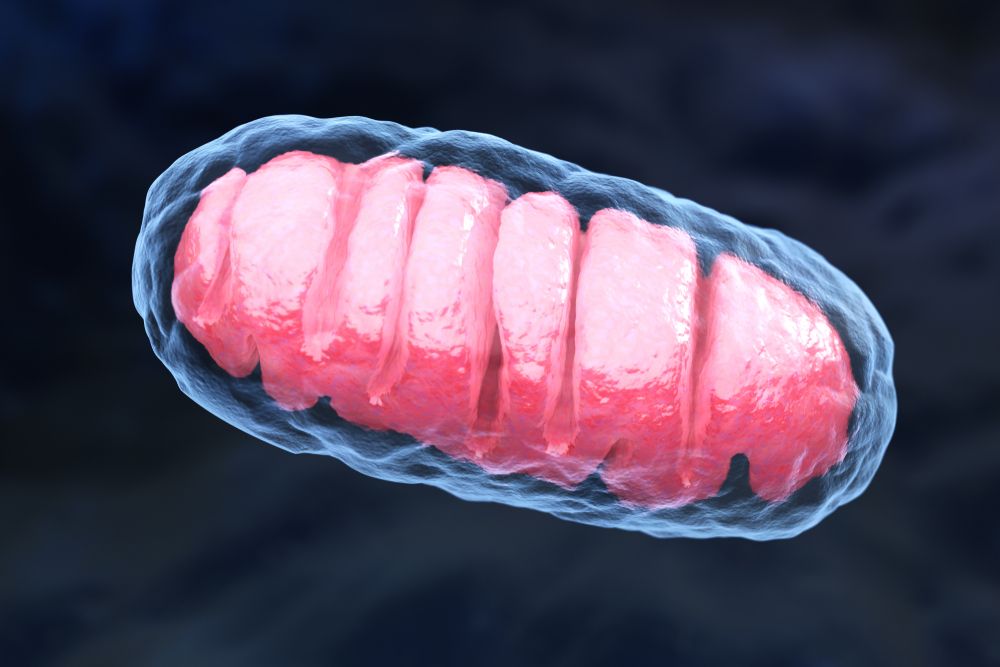
Tatiana Shepeleva/Shutterstock
Abnormalities in cellular transport and in mitochondria (the cell’s powerhouses) are a common feature of motor neurons derived from people with four different subtypes of Charcot-Marie-Tooth disease type 2 (CMT2), a study shows.
Notably, treatment with a suppressor of DLK — a molecule involved in mitochondrial damage and transport inside nerve cells — partially rescued mitochondrial deficits in the two most-affected subtypes.
These findings shed light on the common underlying mechanisms of CMT2 subtypes and highlight the importance of such discoveries in the identification of potential targets and development of new therapeutic strategies for CMT2, the researchers noted.
The study, “Induced pluripotent stem cell-derived motor neurons of CMT type 2 patients reveal progressive mitochondrial dysfunction,” was published in the journal Brain.
CMT2, also known as “axonal CMT,” is characterized by the degeneration of axons — nerve fibers that carry signals to the next nerve or muscle cell — of the peripheral nervous system, which controls movement (via motor neurons) and sensation (through sensory neurons) in the limbs.
This axonal damage leads to gradual muscle weakness and atrophy (shrinkage), as well as reduced sensation — feeling heat, cold, and touch — mostly in the feet, lower legs, hands, and forearms.
CMT2 has been associated with mutations in more than 50 genes, which, together with the high clinical variability across its subtypes, has hindered the development of effective therapies for axonal CMT.
“One of the main reasons for the lag in the development of therapies for CMT2 is that the shared and gene-specific pathways remain largely unresolved,” the researchers wrote.
To address this, a team of researchers in Belgium evaluated whether motor and sensory neurons derived from five patients with the most common forms of CMT2 shared any hallmarks of axonal degeneration.
These included: one patient carrying the R94Q mutation in the MFN2 gene (CMT2A); one with the P8R mutation in the NEFL gene (CMT2E); one carrying the K141N mutation in the HSPB8 gene (CMT2L); and two patients positive for either the G84R or the P182L mutation in the HSPB1 gene (CMT2F).
Notably, these two HSPB1 mutations are associated with distinct disease severity and were included in this study to account for potential variability within the same subtype.
These nerve cells were generated from patient-derived induced pluripotent stem cells (iPSCs) and grown in the lab. iPSCs are generated from fully matured cells that are reprogrammed back to a stem cell-like state, where they can give rise to almost every type of human cell.
As such, when derived directly from patients, these cells can be used as cellular models that mimic the disease’s genetic and clinical diversity. Nerve cells also were derived from iPSCs of two healthy individuals to be used as controls.
Results showed that motor neurons derived from all CMT2 patients exhibited changes in neuronal activity and a trend toward a reduction in neurite network density, reaching statistical significance in the CMT2A and CMT2E subtypes, relative to healthy cells.
Neurites are neuron projections used to communicate with other neurons, and can develop into axons and dendrites.
Motor neurons of all included CMT2 subtypes also showed significantly slower transport of mitochondria and lysosomes across their axons that worsened over time, as well as mitochondria with abnormal shapes, compared with controls.
Lysosomes are cellular organelles involved in the breakdown and recycling of cellular waste.
Further analyses revealed a common mitochondrial dysfunction in all CMT2-derived motor neurons, supported by significant changes in mitochondrial genes’ activity, and impaired mitochondrial function and energy production.
Changes in gene activity also were observed in nerve tissue collected from a mouse model of CMT2L.
Similar abnormalities were found in sensory neurons derived from CMT2 patients with sensory symptoms, while those from CMT2 subtypes with predominant motor involvement (CMT2L and CMT2F) were comparable to healthy sensory neurons.
This supported the “notion that some gene mutations predominantly affect motor neurons,” and demonstrated “that patient-specific motor and sensory neurons recapitulate the disease signatures of CMT2,” the researchers wrote.
Notably, the use of gene editing to correct the MFN2 mutation in iPSCs derived from the patient with CMT2A rescued all the observed abnormalities in both motor and sensory neurons, validating these deficits as “true hallmarks of CMT2A,” the team added.
The researchers then assessed the effects of treating CMT2-derived motor neurons with a suppressor of DLK, an enzyme involved in axonal stress response that is chronically activated in several neurodegenerative diseases.
Previous studies showed that “mitochondrial dysfunction and DLK activation reinforce one another in inducing axonal damage,” and that DLK also is “intimately involved in axonal organelle transport,” the team wrote.
They focused on motor neurons from the patients with CMT2A and CMT2E, since they showed the most severe mitochondrial abnormalities, and found that DLK suppression partially rescued these deficits in both subtypes.
“Altogether, our data reveal shared cellular [features] across different CMT2 subtypes and suggests that targeting such common [disease mechanisms] could allow the development of a uniform treatment for CMT2,” the researchers wrote.






