CRISPR/Cas9 Treatment Can Improve Nerve Functioning in Mouse Model of CMT1A, Study Suggests
Using CRISPR/Cas9 technology to reduce the expression of the gene PMP22 in nerve cells can improve nerve functioning and limit demyelination (damage to the protective covering that surrounds nerve fibers) in a mouse model of Charcot-Marie-Tooth disease 1A (CMT1A), a new proof-of-concept study reports.
The study, titled “Targeted PMP22 TATA-box editing by CRISPR/Cas9 reduces demyelinating neuropathy of Charcot-Marie-Tooth disease type 1A in mice,” was published in Nucleic Acids Research.
CMT1A, which is the most common type of CMT1, is caused by duplication of a region of human chromosome 17. One of the genes in this region is PMP22 (peripheral myelin protein of 22 kDa), which encodes for a protein of the same name. It is thought that this duplication leads to too-high levels of PMP22 protein, which in turn helps drive demyelination or the loss of myelin (the protein “sheath” around neurons that helps them function correctly) in CMT1A.
Based on this idea, researchers behind this study wanted to develop a method by which they could lower PMP22 expression. They turned to the CRISPR/Cas-9 system, which allows researchers to alter certain specific sequences of DNA.
The particular region the researchers decided to target was the TATA-box of PMP22. The TATA-box is a sort of “start” signal for the molecules that “read” DNA — kind of like how capital letters can indicate the start of sentences. The basic idea is that, by removing this sequence, the DNA-reading machinery will not be able to read the PMP22 gene, which will ultimately result in less PMP22 protein being produced by a cell.
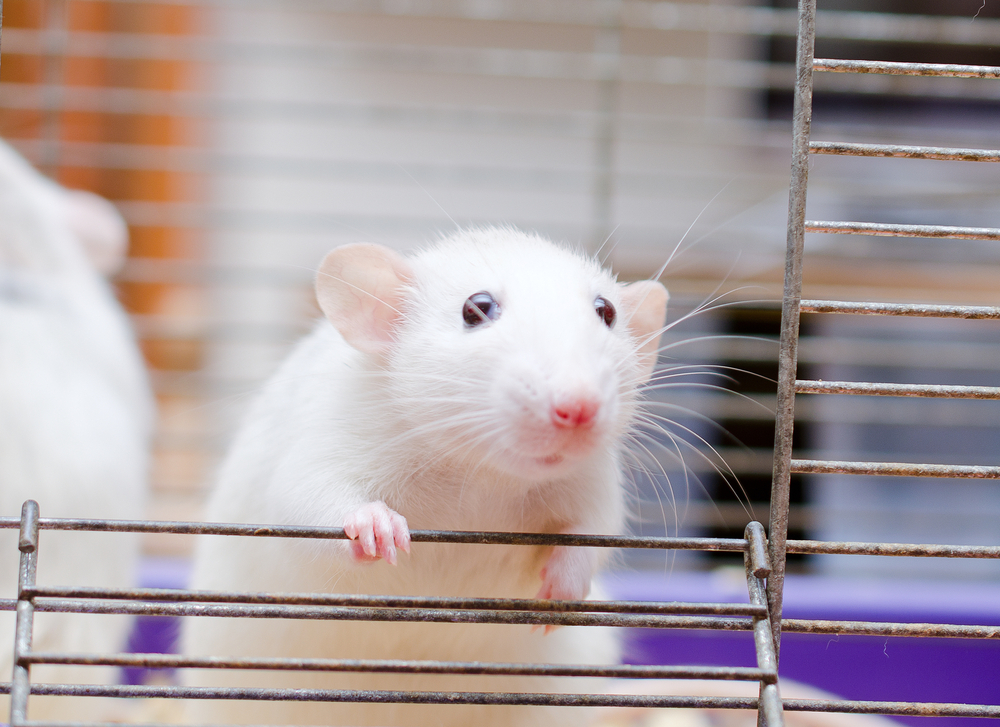
The researchers first tested this strategy using cells in dishes. They confirmed that their system was targeting the right region, and that this targeting resulted in lower levels of PMP22. Then, they turned to a mouse model of CMT1A — C22 mice, which has multiple copies of human PMP22.
The researchers used their system on one of the sciatic nerves (the nerve that stretches from the hip to the feet) of these mice, with the same nerve on the opposite side of each mouse’s body being used as a control.
The researchers confirmed that nerves targeted in such a way had significantly decreased expression of PMP22 — 44.64% less than controls, on average. Additionally, they found that these nerves had more myelin than untreated nerves, indicating the strategy’s intended effect.
Importantly, these findings were based on CRISPR/Cas9 administration six days after the mice were born, which the researchers noted could be a preventive measure rather than treatment and would limit the utility of this strategy in a clinical setting.
So, they tested the system on three-week-old mice. They found that these mice had similar decreased PMP22 expression (by 40.67% on average), and myelin was also increased in treated nerves of these older mice. Plus, the researchers determined that treated nerves in these mice worked better than untreated ones, as evidenced by increased motor nerve conduction velocity and compound muscle action potential. Basically, the treated nerves were better at signaling electrical signals.
Importantly, the researchers also sequenced the genomes of treated cells to look for evidence of off-target effects (that is, regions of DNA that were changed even though they weren’t supposed to be), which are a major concern when using “gene editing” technologies such as CRISPR/Cas-9. The researchers didn’t find any of these effects, suggesting that there were none or so few that none were detected.
“In summary, our data demonstrate the proof-of-principle for PMP22 downregulation via CRISPR/Cas9 targeting TATA-box of the PMP22 promoter region,” the researchers said. “Therefore, CRISPR/Cas9-mediated modification of the TATA-box of PMP22 promoter holds promise for the treatment of CMT1A.”