Study Sheds New Light on How HARS1 Mutations Cause CMT in Cells, Zebrafish
Mutations in the gene HARS1, which are a cause of Charcot-Marie-Tooth disease (CMT), result in reduced protein production in neurons — providing a possible mechanism for how these mutations cause disease — a recent study found.
The findings were published in The FEBS Journal, in a study titled “Neuropathy‐associated histidyl‐tRNA synthetase variants attenuate protein synthesis in vitro and disrupt axon outgrowth in developing zebrafish.”
CMT, a group of inherited disorders of the peripheral nervous system, can result from mutations in many different genes. Defining exactly how a given mutation leads to disease is important for understanding the disorders and provides a foundation for the future development of therapies.
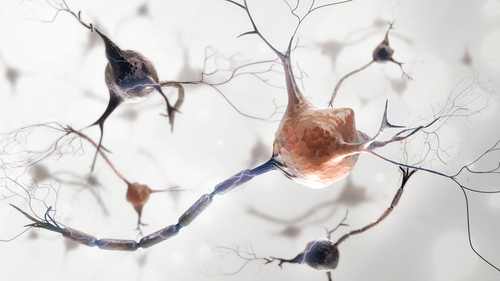
One group of genes that has been implicated in CMT are the aminoacyl-tRNA synthetases (ARSs). The proteins encoded by these genes are important for the attachment of transfer RNA (tRNA) to amino acids — a critical early step in the production of proteins. In addition, ARSs have been implicated in other functions, including regulating immunity and blood vessel growth.
It remains unclear exactly how ARSs affect cells, particularly neurons, in CMT. Further, the exact consequences to the rest of the nervous system from these changes within the cells also are not well understood.
To learn more, a team of researchers assessed three CMT-associated mutations — named V155G, Y330C, and R137Q — in the gene HARS1, one of the 37 ARS genes in the human genome. First, the scientists analyzed these mutations using the rat cell line PC12 in dishes.
When neurons grow, they produce long extensions used for communication with other neurons, which are called neurites. Compared with cells with a normal HARS1 gene, cells with CMT-associated HARS1 mutations had the same number of neurites; most of the neurites were the same length. However, the longest neurite on a given cell — which would typically develop into an axon in the context of a living animal — was significantly shorter in cells with mutant HARS1.
“The results of these experiments suggest that the principal phenotypic consequence of overexpression of CMT-HARS1 mutants in the context of differentiating PC12 cells is shortening of the longest neurite,” the researchers wrote.
The team then treated cells with chemicals that blocked the activity of the HARS1 protein, or blocked protein synthesis generally. These treatments led to similar results as having the mutant protein. That suggests that the mutations result in smaller neurites by making HARS1 function abnormally, specifically in terms of protein synthesis.
Reduced functionality is the most common consequence of mutations, but some mutations can instead give proteins additional, toxic functions. Thus, it is always necessary to check.
Further experimentation with the PC12 cells confirmed that those with HARS1 mutants had significantly reduced protein synthesis and significantly increased levels of eIF2 alpha, a marker of cell stress.
“Thus, the neurite outgrowth defects described earlier are likely to be the result of decreased protein synthesis, which appears to be linked to induction of the [cell stress response],” the researchers concluded.
Such mutations in zebrafish were next evaluated to validate these cellular findings in living animals. Consistent with the cell data, zebrafish with mutant HARS1 had significantly shortened axons. Zebrafish with mutant HARS1 also behaved abnormally, such as being less responsive to touch. As in the cells, treatment of zebrafish with a chemical that blocks protein synthesis led to similar effects.
“The effects on neurite outgrowth observed in PC12 cells were faithfully recapitulated in a zebrafish model of neuronal development,” the researchers wrote.
Like many ARS proteins, HARS1 functions as a dimer – that is, two individual HARS1 proteins working together to carry out the protein’s function. In a final set of experiments, the researchers used cells in dishes to demonstrate that mutant HARS1 proteins could form dimers with the normal HARS1 protein.
This finding provides a possible explanation for ARS mutations that are dominantly inherited, in which only one mutant gene is sufficient to cause disease. Of note, each individual inherits two copies of each gene, one from each parent.
Specifically, the findings suggest a dominant negative mechanism, where the mutant protein makes the normal protein work abnormally. Essentially, the idea is that if mutant HARS1 and normal HARS1 form a dimer, the dimer as a whole will not be able to function, even though half of it is normal protein.
Overall, this study sheds new light on some of the molecular mechanisms underlying CMT. It lays the foundation for further investigations that could eventually lead to new treatments for disorders affecting the peripheral nervous system.
“Going forward it will be essential to test whether zebrafish overexpressing CMT-ARS mutants exhibit the same types of neuromuscular junction deficits seen in mouse models,” the researchers wrote.





