Changes in Sciatic Nerve of Thigh May Reflect Disability in CMT1a Patients
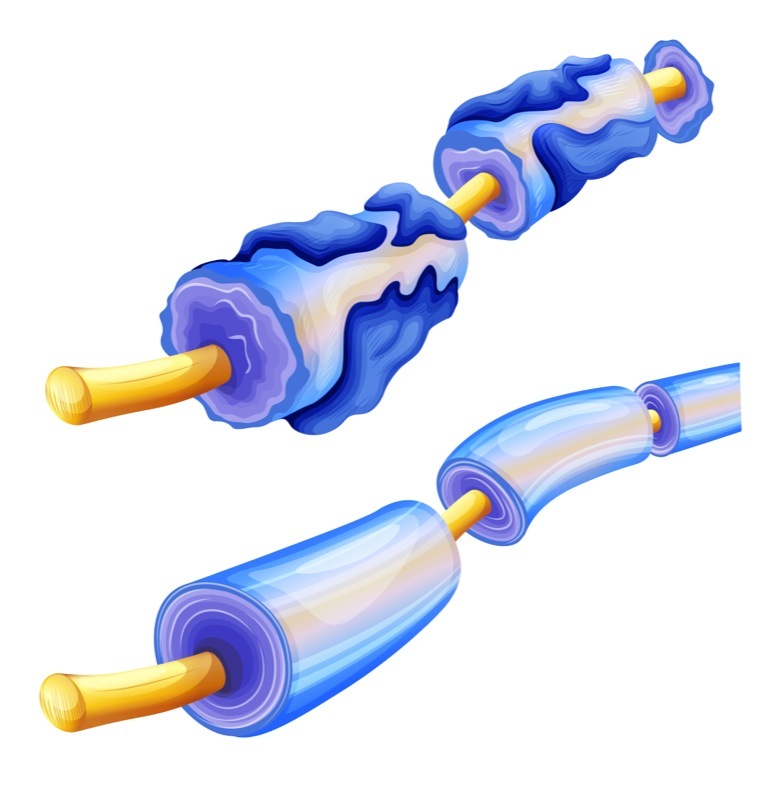
Changes to nerve tissue in the thigh appear to relate to clinical disability in people with Charcot-Marie-Tooth disease type 1a (CMT1a), and may be used to assess the disease’s natural progression and the effectiveness of treatment approaches, a study in patients suggests.
The study, “Quantitative assessment of sciatic nerve changes in CMT1A patients using magnetic resonance neurography,” was published in the European Journal of Neurology.
Researchers then investigated whether there was an association between any of these measures in the thigh or leg with other measures of clinical disability, such as muscle strength — assessed via the Medical Research Council, or MRC — and disease severity, using the Charcot Marie Tooth examination score (CMTES) alone or a version that includes electrophysiological testing (CMTES version 2).
Functional disability in daily life was measured through the overall neuropathy limitation scale (ONLS) and its lower limb subpart (ONLSL).
Statistical analysis demonstrated that nerve volume in the thigh significantly correlated with all clinical measures, but that was not seen for the tibial nerve volume.
The proton density in the sciatic nerve also significantly correlated with both measures of functional disability, and the magnetization transfer ratio in this nerve related to muscle strength in the quadriceps.
Only the magnetization transfer ratio in the leg nerve correlated significantly with ONLS, but no other measures of nerve damage in the tibial nerve associated with clinical scores.
The findings “highly suggest that [qMRI] measurements at the thigh level might be the most appropriate in order to assess both the natural disease progression and the potential efficiency of therapeutic strategies,” the researchers wrote.
Still, these nerve tissue measures need to be further characterized to understand how they change over time, and whether they accurately reflect disease progression and response to treatment in patients.
“The sensitivity of the selected metrics would have to be assessed through repeated measurements over time during longitudinal studies to evaluate structural nerve changes under treatment,” the team concluded.





