Mitochondrial Gene Mutation Linked to CMT in Large Venezuelan Family
Written by |
Mutations in a mitochondrial gene that does not code for a protein have been implicated, for the first time, in the development of Charcot-Marie-Tooth (CMT) disease.
These gene mutations were found in a large, indigenous Venezuelan family with more than 3,700 living members, nearly 100 of whom have experienced CMT-related symptoms.
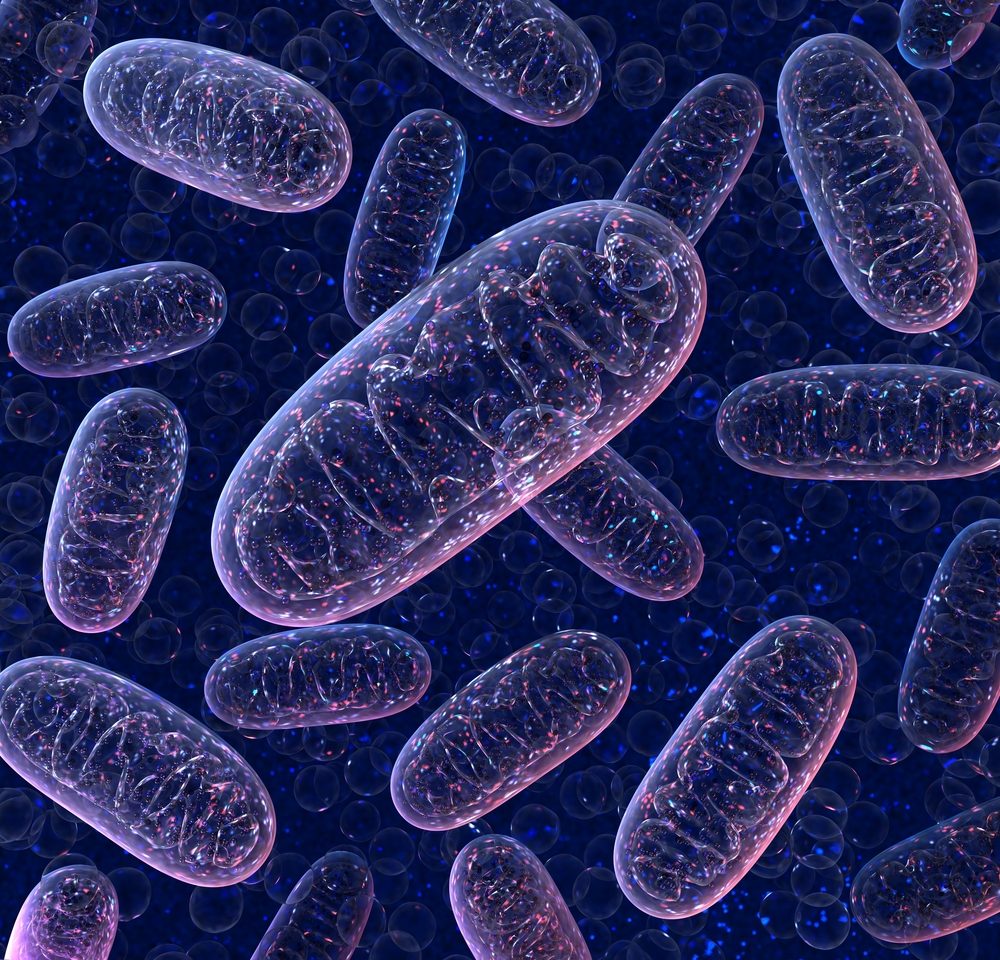
According to the investigators, this is the second gene in the mitochondria — the powerhouses of cells — to be associated with the disease so far. These findings highlight the diversity of the genetic causes that lead to CMT.
The study, “A Mitochondrial tRNA Mutation Causes Axonal CMT in a Large Venezuelan Family,” was published in the journal Annals of Neurology.
More than 100 genes have been associated with CMT development. Among them, all code for a certain protein, and the vast majority are found in the DNA in the cell nucleus.
However, mitochondria — cellular compartments that work as energy-producing factories in cells — have their own set of genes, and a mutation in a mitochondrial protein-coding gene also has been implicated in CMT.
Now, researchers based in the U.S. and Venezuela identified a new mitochondrial gene that also is associated with CMT. But unlike all the other genes associated with the disease, it did not code for a protein.
The gene was found in a large family with axonal CMT whose inheritance pattern was consistent with a mitochondrial mutation — specifically, mother to child.
The axonal form of CMT causes the degeneration of peripheral nerve axons that connect the brain and spinal cord to the rest of the body. Most patients with axonal CMT lack a genetic diagnosis.
This family had more than 3,722 living members from 11 branches, including 97 individuals — 55 female and 42 male — who had CMT-associated symptoms and had been diagnosed with clinical neuropathy, or nerve disease.
Originally the family came from a single village in the Sucre municipality, Mérida state.
Investigators assessed 44 of the 97 patients, who had a mean age of 41.1 years; their clinical symptoms started around the mean age of 15.3, though the onset ranged from ages 1 to 68.
Most of the patients experienced muscle weakness and wasting in the legs and feet, along with a loss of muscle coordination. In all, 31 were still able to walk without any aid. Six required a cane to walk and two a walker, while five needed a wheelchair.
Of the 22 individuals who had gait impairments, 18 showed signs of axonal damage in both motor and sensory neurons, with sensory nerves being more severely affected than motor nerves.
In all 97 cases, the affected individuals inherited the disease from the maternal line, consistent with a mitochondrial inheritance pattern. Of note, people inherit mitochondria only from their mother and not from their father.
Mitochondrial DNA sequencing in three affected family members and one asymptomatic carrier revealed a mutation, called m.1661A>G, located in the mt-tRNAVal (MT-TV) gene. Instead of originating a protein, this gene codes for transfer RNA — a form of RNA that carries amino acids to be included in the sequence of proteins.
Interestingly, multiple large, unrelated mutations were detected in the affected individuals, but not the asymptomatic carrier.
The researchers performed whole-exome sequencing — assessments to find the genetic cause of disease symptoms — on four family members, three affected and one clinically unaffected carrier.
Analysis of muscle tissue from these four relatives revealed signs of both muscle denervation and reinnervation. Denervation is the loss of nerve connections to the muscle fiber, while reinnervation is the restoration of nerve connections after such loss.
Notably, reinnervation was more pronounced in the more severely affected patients than it was in the mildly affected or asymptomatic individuals.
Moreover, nerve biopsies from two of the affected family members showed mitochondrial abnormalities that were consistent with nerve damage resulting from mitochondrial problems.
Decreased activity also was found among mitochondrial proteins that are needed to produce energy. But this was much more prominent in severely affected patients compared with an unaffected individual or a patient with mild symptoms.
A severe reduction in MT-TV levels also was found in the muscles of affected individuals. Similar to nerve damage, the change in MT-TV levels was more pronounced in more severely affected family members. A corresponding increase in a different gene, called mt-tRNAPhe, may help compensate for that reduction.
The findings “suggest that mtDNA sequencing can be considered for patients with CMT without a genetic diagnosis, even if no other features of mitochondrial disease are present,” the researchers wrote. They note that further studies are needed to clarify the exact mechanism through which the m.1661A>G mutation leads to the condition.
Among the study’s limitations, according to the investigators, are the potential of non-CMT related causes of neuropathy, the limited access to genetic material and tissue samples from the family, and the possibility that a different mutation may contribute to the observed neuropathy.





