JAG1 Gene Mutations May Lead to Peripheral Nerve Damage Linked to CMT2, Study Reports

Mutations in the Jagged1 (JAG1) gene may compromise the integrity of peripheral nerves — those found outside the brain and spinal cord — and lead to peripheral neuropathy associated with Charcot-Marie-Tooth disease type 2 (CMT2), a study reports.
The study, “Dominant mutations of the Notch ligand Jagged1 cause peripheral neuropathy,” was published in The Journal of Clinical Investigation.
The Notch signaling pathway plays a key role in tissue development and cell fate. Dysregulation of this signaling cascade has been shown to lead to several diseases, including cancer and developmental syndromes.
The JAG1 gene encodes a protein that works as a ligand and activator of the Notch pathway. Now, investigators in the U.S. and U.K. have discovered that mutations in this gene may lead to the onset of CMT2.
In the study, they examined individuals who had been diagnosed with CMT2 from two unrelated families. Patients had vocal fold paresis — loss of control over their vocal cords due to nerve damage — and mild limb weakness.
A genetic analysis of three members with CMT2 from one of the families showed that they all carried a genetic variant (c.1731C>G) in a region of the JAG1 gene. CMT2 patients in the second family also carried a genetic variant (c.1948T>C) in the same gene.
The newly identified genetic variants caused changes in the amino acids (the building blocks of proteins) of JAG1 that computer analyses estimated would likely affect the function of the protein. Structural modeling also predicted these amino acid alterations might affect the region of JAG1 that interacts with the Notch receptor, “raising the possibility that [these] mutations could disrupt [ligand-receptor] interaction.”
The researchers then performed a series of experiments in cells cultured in a lab dish to investigate how these mutations might alter the normal function of the JAG1 protein.
In their experiments, they introduced each of the mutated proteins into cells and saw that both were located at the cell’s membrane, albeit at lower levels compared to the normal JAG1 protein.
This was because both mutated proteins were also found inside cells in an organelle, called the endoplasmic reticulum (ER), which is responsible for producing and modifying proteins. Their retention at the ER led to a reduction of their levels at the cell surface compared to control cells that produced the normal protein.
Previous studies have suggested that JAG1 needs to undergo a modification process, called glycosylation. This modification, which adds sugar molecules to the protein (glycans), is thought to be required for JAG1 to be taken to the cell’s surface. This led researchers to investigate if the new mutations changed the glycosylation pattern of JAG1.
Their experiments confirmed that these mutations significantly reduced the glycosylated form of JAG1, which might also explain why these mutant proteins were found at lower levels at the cell’s surface.
Next, the researchers explored how these molecular alterations in the JAG1 protein could be linked to neuropathy using mice that had been genetically modified to carry the same mutation found in CMT2 patients from one of the families (c.1731C>G; p.Ser577Arg).
They found that when mice carried two copies of the mutated Jag1 gene, they died before birth. Conversely, animals carrying one healthy and one mutated copy of the gene (heterozygous mice) completed embryonic development and were born, but showed motor and behavior alterations later in life.
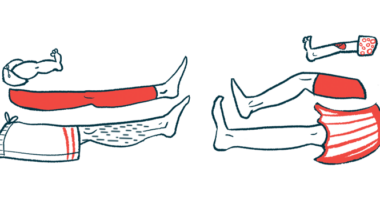
The inverted grid test (a test that measures how long animals can cling to a surface while upside down) showed that mutated mice had less limb strength compared to healthy animals (controls).
Yet, in the rotarod test — a test that measures balance while animals are running on a moving rod — no differences were found between mutated and control mice. Between 19 and 23 months of age, these mice showed a reduction in the compound muscle action potential, which is a test that measures muscle electric activity.
When investigators examined the animals’ recurrent laryngeal nerve, which controls larynx muscles, they found no morphological alterations. Yet, there was an increase of focally folded myelin (the protective sheath that covers nerves). This abnormality in peripheral nerves has been observed in different forms of heredity neuropathy and aging, suggesting that these mice had a mild form of peripheral neuropathy.
Overall, “our clinical, genetic, biochemical, and mouse model findings implicate JAG1 mutations as a cause of CMT2 with severe vocal fold paresis,” the researchers wrote.
“[They also] highlight a critical role for JAG1 in maintaining peripheral nerve integrity … and provide a basis for the evaluation of peripheral neuropathy as part of the clinical development of Notch pathway-modulating therapeutics,” they added.