Gene Therapy for CMT4C Fares Well in Preliminary Tests in Mice
A gene therapy strategy to treat Charcot-Marie-Tooth disease 4 subtype C (CMT4C), targeted to correct the myelin-producing cells of the peripheral nervous system, showed positive results in a mouse model.
The data provide proof-of-principle support for gene therapy to treat CMT4C and potentially other similar demyelinating inherited nerve diseases.
The findings appeared in the report “Gene replacement therapy in a model of Charcot-Marie-Tooth 4C neuropathy,” published in the journal Brain.
In this study, researchers sought to explore the potential of gene therapy as a treatment for CMT, a genetic disease caused by defects in the function of peripheral nerves — the nerves that control movement (motor nerves) and our senses (sensory neurons).
They focused particularly on CMT4C, which is caused by mutations at the SH3TC2 gene. Through unclear mechanisms, defects in this gene result in damage to the myelin sheath, the insulating fat-rich protective layer that surrounds nerve fibers.
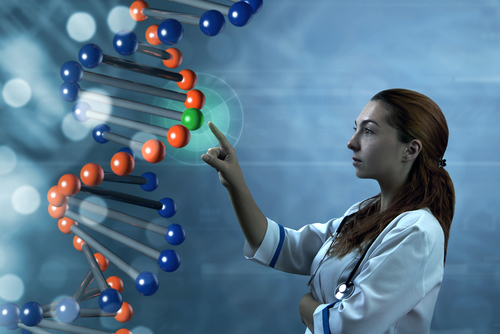
SH3TC2 instructs for the production of a protein of unknown function, which appears to be particularly enriched at and important to the myelin-producing cells of peripheral nerves, called the Schwann cells.
Researchers took advantage of a well-characterized mouse model to study this type of CMT. This model is unable to produce the SH3TC2 protein and has several features of the human disease, such as early progressive loss of myelin and slowing of nerve conduction velocities.
The gene therapy technique chosen was based on a viral vector called lentivirus. Researchers used a modified lentivirus (with no capacity to replicate and cause an infection) to deliver a functional copy of the human SH3TC2 gene into nervous system cells. The engineered gene had the capacity to produce a fully working SH3TC2 protein.
They devised a strategy to ensure that this gene copy was primarily turned on at the Schwann cells, placing the corrected gene under the control of a DNA sequence only active in those cells.
Gene therapy was administered to mice by injection into the spinal canal (intrathecal injection). Four to eight weeks after the treatment, several measurements to assess response to therapy were taken.
The treatment led to widespread rescue of SH3TC2 in Schwann cells. The protein became expressed at sciatic nerves and lumbar nerve roots (where nerves branch off from the spinal cord), as well as other tissues of the peripheral nervous system.
Treatment of three-week old mice improved the animals’ motor ability and the speed of motor nerve conduction, increased the fraction of myelinated fibers and the thickness of myelin layers, compared to placebo-treated animals.
Treated mice also had lower blood concentrations of neurofilament light chain protein (NfL), a clinically relevant biomarker of neuronal injury.
“Thus, our study provides a first proof of principle for viral gene replacement therapy targeted to Schwann cells to treat CMT4C,” researchers said.
The team proposes that other demyelinating neuropathies that result from mutations in a Schwann cell-specific gene may also benefit from this type of approach.
“Further studies are needed to optimize vector safety and biodistribution, gene expression levels, as well as to demonstrate effectiveness of this approach after the onset of neuropathy, in order to facilitate the clinical translation for CMT4C patients,” they said.