MRI-based Technique Enables Early Diagnosis of Sciatic Nerve Damage in CMT1 Patients, Study Reports
A technique called diffusion tensor imaging (DTI) enables diagnosis of sciatic nerve damage in patients with Charcot-Marie-Tooth disease type 1 (CMT1).
The study, “Diffusion tensor imaging of the sciatic nerve in Charcot-Marie-Tooth disease type I patients: a prospective case-control study,” appeared in the journal European Radiology.
The use of imaging techniques may help CMT diagnosis, which often goes unrecognized before the presentation of overt clinical symptoms. Changes in the peripheral nerves of CMT patients, and quantitative analysis of imaging measures have received little attention, despite reports of nerve hypertrophy (enlargement) and muscle alteration due to denervation in these patients.
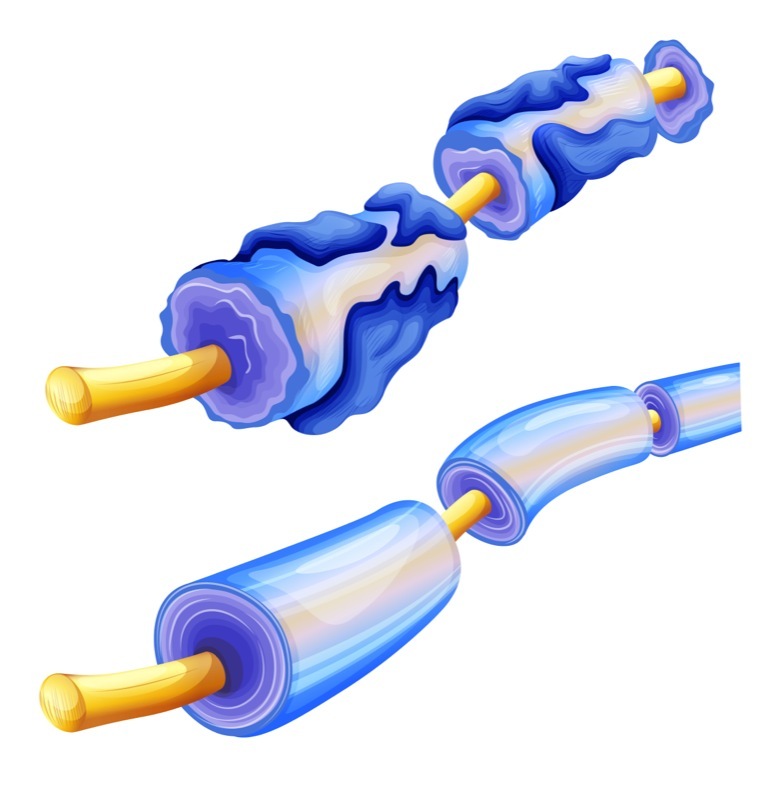
DTI is an increasingly used magnetic resonance imaging (MRI)-based technique, reported to have potential in assessing nerve degeneration and regeneration. Among DTI parameters, previous studies suggested that axial diffusivity (AD) and radial diffusivity (RD) — which represent parallel or perpendicular diffusion of water relative to nerve fiber — may have high clinical value. These parameters have been reported to reflect the integrity of nerve fibers and of their protective layer, called myelin.
In the study, a research team from Korea conducted prospective research to evaluate whether DTI parameters may reveal the difference between demyelinated (myelin loss) sciatic nerves in CMT1 patients, and normal sciatic nerves of healthy controls, and, therefore, have diagnostic value for CMT1. The investigators also hypothesized that the cross-sectional area (CSA) of the sciatic nerve is different between patients and controls.
A total of 18 CMT1 patients (8 men and 10 women, with a mean age of 30.1 years, and age range from 23 to 37 years) underwent MRI scans between February and June 2017. The investigators selected young adults so as to include patients still at an early stage of CMT1. All 17 patients who underwent genetic testing were diagnosed with CMT1A (one patient who did not undergo genetic testing was diagnosed with CMT1, based on clinical history and electrophysiologic study results).
Eighteen controls — with no history of peripheral neuropathy (peripheral nerve damage) or conditions related to the lower extremities — were also included in the study.
DTI images were obtained from the anterior inferior iliac spine — a bone prominence on the border of the hip bone — through the distal femur, just above the knee joint. Analysis was performed at four levels from the hamstring tendon origin through the mid-femur.
The results revealed that fractional anisotropy (FA) — a measure of the degree of variation in diffusion asymmetry — was significantly lower at all four levels in CMT1 patients than in controls. In contrast, CSA, RD and mean diffusivity — a combination of AD and RD — were significantly higher at all four levels in CMT1 patients. AD was significantly higher at level 2 (in the femur) in CMT1 patients.
According to the team, the different CSA of the sciatic nerve in CMT1 patients may be due to disease hallmarks, such as loss of myelin or fibrosis (scarring) around the myelin sheath.
“These results may imply a feasibility for clinical application of DTI in the evaluation of the sciatic nerve in CMT type I patients and, possibly, in patients with other types of demyelinating neuropathy,” the investigators wrote. “The CSA of the sciatic nerve is also a potential parameter for diagnosing nerve abnormality in CMT type I patients.”
Among the study’s limitations, the researchers mentioned the low number of patients, and not testing the correlation between neurologic symptoms and imaging parameters.