Schwann Cells Discovery May Be Good News for CMT Research
Written by |
New findings suggest that Schwann cells are able to make the protective layer myelin for multiple nerve cells. This discovery goes against conventional wisdom about how Schwann cells work, and it could have major implications for our understanding of peripheral neurodegenerative diseases, including Charcot-Marie-Tooth disease (CMT).
The study with that finding, “Myelinating Schwann cells ensheath multiple axons in the absence of E3 ligase component Fbxw7,” was published in Nature Communications.
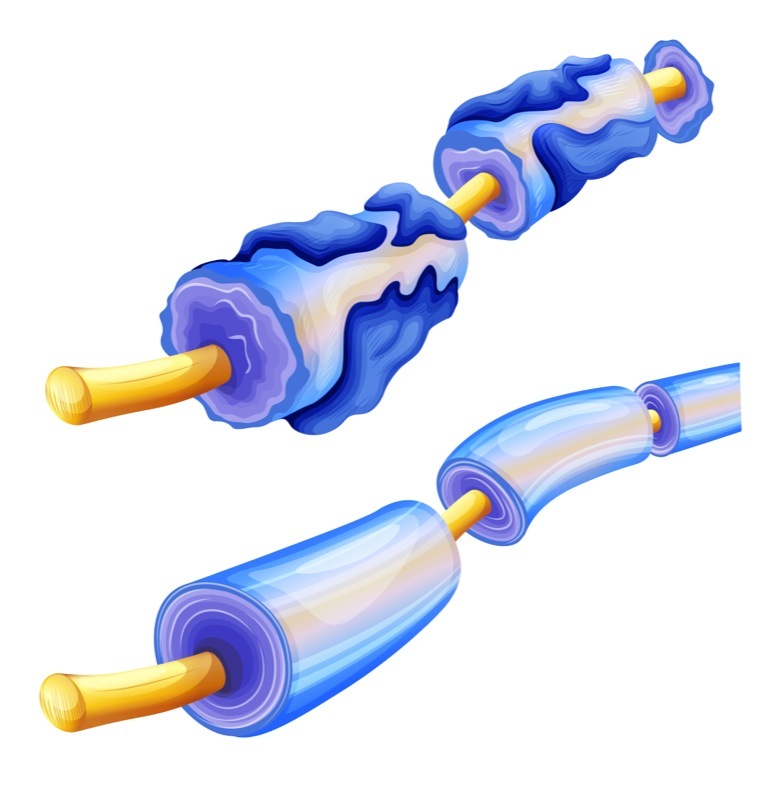
Myelin makes up the sheath that envelops axons, which are the protrusions neurons use to send electrical signals to each other. This sheath allows the cells to send their signals more efficiently, and when it’s damaged — as in the most common type of CMT, CMT1 — it can cause serious problems.
But not all myelin in the body is made in the same way. Specifically, there are two types of myelin-making cells: oligodendrocytes and Schwann cells.
Oligodendrocytes are responsible for putting myelin in the central nervous system (the brain and spinal cord), and they can put myelin around multiple different axons. Schwann cells put myelin in the rest of the body (the peripheral nervous system, which is damaged in CMT).
Until now, it has been thought that Schwann cells lack the multi-exon-myelinating capabilities of oligodendrocytes; the prevailing understanding has been that one Schwann cell puts myelin on one axon. However, this new study reveals that isn’t the case, at least not in some (fairly specific) circumstances.
The researchers’ discovery began in zebrafish. They noticed that fish with a mutation in a particular gene, fbxw7, had more myelin than expected.
The investigators then engineered mice whose Schwann cells lacked functional fbxw7, and they made an unexpected discovery: the mutant Schwann cells appeared to be putting myelin on multiple axons at once, the very trait that was thought to be exclusive to oligodendrocytes.
“This totally overturns the textbook definition of the way Schwann cells work,” Kelly Monk, PhD, a professor at Oregon Health & Science University and co-author of the study, said in a press release. “It highlights a very plastic [changeable] potential for these cells.”
It’s important to note that this change didn’t make the mice’s nervous systems work better. Indeed, mice with the fbxw7 mutation displayed slight, but significant, motor deficits compared to wild-type mice. But the fact these cells can do this at all opens up new avenues for scientific exploration and, perhaps, treatments for when these processes become dysregulated.
It remains unclear exactly how this particular genetic change confers increased myelinating activity, but knowing these cells exhibit this plasticity at all may be indicative of different evolutionary pressures faced by cells in the central and peripheral nervous systems.
The researchers speculated that, in the peripheral nervous system, it is relatively common for there to be damage that the organism as a whole can survive. So, there would be an evolutionary pressure for cells that can be flexible to help repair the damage. In contrast, “There’s no selective pressure in repairing myelin damage in the central nervous system, because you’re probably going to die,” Monk explained.
It remains to be seen whether this myelin-making ability could be exploited or manipulated to help treat neurodegenerative diseases like CMT. Further research will be needed. But, Monk speculated, “Targeting the fbxw7 gene — or downstream pathway molecules — could be a powerful way to promote myelin repair.”





