Study Links Eight Genes in Skin to Severity and Progression of Charcot-Marie-Tooth Disease
Written by |
Eight genes in the skin of patients with Charcot-Marie-Tooth disease correlated with the severity and progression of the disorder, a study reports.
The research, which applied to Charcot-Marie-Tooth disease type 1a (CMT1a), suggested that the genes could be used as biomarkers of treatments’ effectiveness, including in clinical trials.
Titled “Biomarkers predict outcome in Charcot- Marie-Tooth disease 1A,” the study was published in the Journal of Neurology, Neurosurgery, and Psychiatry.
CMT1a is the most common inherited nerve disorder. It usually shows up in the first two decades of life, with symptoms that include foot deformities and walking disabilities. But it can manifest itself and progress in many ways, even between twins.
The cause of more than half of CMT1a cases is a mutation in the gene coding for PMP22, a protein that, when normal, plays a role in the development of the myelin sheath that protects nerves. When it’s abnormal, it is associated with damage to the sheath.
Biomarkers of the disease’s severity and progression would help researchers do a better job of evaluating CMT1a treatments in clinical trials, researchers said.
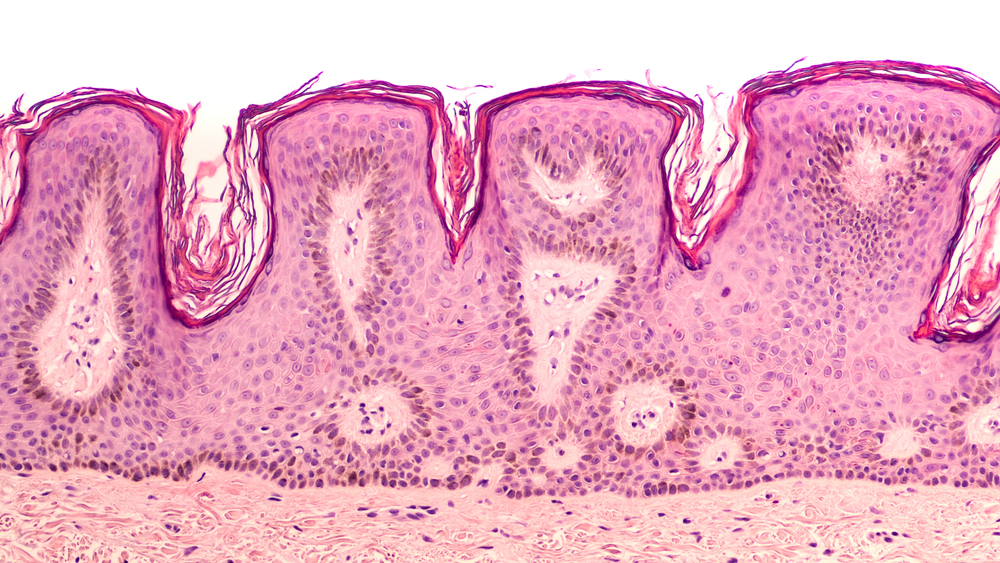
A previous study that the team did with a rat model of CMT1A suggested that genes found in human skin biopsies might be good biomarkers of the severity and outcomes of the disease. The level of the biomarkers correlated with patients’ impairment, the research suggested.
In a follow-up study, the team looked at skin biopsies of 46 CMT1A patients that were introduced to a rat model of the disease. They found messenger RNA, or transcripts that genes use to create a protein, in the rats.
The researchers decided to try to confirm their findings by looking for 16 CMT rat-derived biomarkers. They examined skin biopsies from 266 CMT1A patients taken at nine centers in the United States and Europe.
They found significant correlations between eight of the skin genes – CDA, CTSA, GRIA1, ENPP1, ANPEP, FN3KRP, GSTT2 and PPARG – and the severity of the disease.
“Given the poor detectability of clinical impairment over time, disease progression biomarkers could markedly accelerate the development of a therapy,” they wrote.
The team then looked at the 16 genes in a second set of skin biopsies collected two to three years later. This collection covered 45 of the original 266 patients.
They discovered that the expression of six genes — PPARG, GSTT2, CTSA, CDA, ENPP1 and NRG1-I — changed over time, correlating with the progression of the disease. Expression is the process by which information from a gene is used to create a functional product like a protein.
Overall, “we provide evidence that cutaneous [skin messenger RNA] transcripts in patients with CMT1A serve as disease severity and progression biomarkers and, if implemented into clinical trials, they could markedly accelerate the development of a therapy for CMT1A,” the researchers concluded.





